There is growing literature about the positive and moderating roles that parent-child relationships can have for adolescent and adult mental health outcomes. Research has shown, for example, that positive and communicative parent-adolescent relationships significantly predict lower adolescent depressive symptoms and can moderate negative effects of parental conflict in families (Ackard et al., 2006; Morgan et al., 2012; Osborne & Fincham, 1996). Many of these studies use population-level data sets and control for families’ racial and ethnic identity. In doing so, much of this literature implicitly assumes the framework of the standard North American family, allowing the largest population to guide the results and assuming that racial and ethnic identity merely adjusts the relationship between parent-child relationships and adolescent mental health (Smith, 1993). Rather than understanding how emotional and relational aspects of families may function differently by family race and ethnicity, the largest populations are centralized.
In addition to large-scale population-based studies, there is also a range of literature about the specific ways that race and ethnicity structure and have meaning for parent-child relationships and family mental health outcomes (Davidson & Cardemil, 2009; Smith & Sun, 2014). Scholars have found that parent-child relationships can moderate the negative effects of racism and discrimination on adolescent mental health for Black families in the United States, that parent-child relationships hold specific gendered meanings for Latinx families where children participate in language brokering for immigrant parents, and that the relationships between family-child relationships and child mental health vary by race and ethnicity (Cooper & McLoyd, 2011; Love & Buriel, 2007; Moon & Rao, 2010).
In this project, we expand on current research about race, parent-child relationships, and adolescent mental health by evaluating race and ethnicity as central structuring forces in family processes rather than using racial identity as a control or assuming that the way white middle-class families live their lives is the “best” or most “normal.” In thinking about race as a structuring force in families (which has negative effects for mental health), this includes acknowledging the role of racism as both a structural force and as an interpersonal reality for families of color. We use stepwise-regression analysis to understand these relationships and focus on what these relationships look like in adulthood.
Research Questions
We address the following research questions: How does mental health vary by race/ethnicity in adulthood? How do parent-child relationships, specifically maternal closeness and living arrangements, shape mental health across race/ethnicity in adulthood?
Methods
Data
To complete the analyses proposed, we use data from the National Longitudinal Study of Adolescent to Adult Health (Add Health), Waves I, IV, and V. Add Health is a nationally representative, school-based sample of respondents who were in the 7th through 12th grades from 1994–1995 in the United States and were followed until they were ages 32–42 years old in 2016–2018 at Wave V, the most recent Wave of data collection. At Wave IV, respondents were 28–34 years old. More information about the data is available at https://addhealth.cpc.unc.edu/. We restricted the analytic sample to individuals who completed Waves I, IV, and V, had valid cross-sectional sample weights at Wave V, and did not have missing data on the dependent variable, independent variables, and control variables. This led to an analytic sample of 8,970 respondents.
Measures
Dependent Variable
Depressive symptoms at Wave V were based on the Center for Epidemiologic Studies Depression Scale (CES-D) and included the following items asked of the respondent in the past seven days at the time of interview: “I felt like I could not shake off the blues, even with the help from my family and friends”; “I felt depressed”; “I was happy” (reverse-coded); “I felt sad”; “I felt that life was not worth living.” Items ranged from never or rarely (1) to most of the time or all of the time (4).
Primary Independent Variables of Interest
The primary independent variables of interest included maternal closeness, parent-child living arrangements, and race and ethnicity. Maternal closeness was measured at Wave IV and included the respondent’s answer to the following question: “How close do you feel to your mother figure?” Answers ranged from 1 (not at all close), 2 (not very close), 3 (somewhat close), 4 (quite close), to 5 (very close). Parent-child living arrangements at Wave IV included whether the respondent was living with their parents or not at Wave IV. Race and ethnicity was measured at Wave V and included non-Latinx Black, Latinx, non-Latinx Asian, and non-Latinx white categories.
Controls
We included the following controls, including gender (male or female), maternal education in adolescence (did not graduate high school and less; high school graduate or GED; some college; completed college and more), and family structure in adolescence (two biological parents; two parents; single parent; and other).
Analytic Approach
To complete the analyses, we first conducted weighted summary statistics of the analytic sample. Then, we conducted summary statistics by race and ethnicity for depressive symptoms at Wave V. Finally, we conducted stepwise OLS regressions with the primary independent variables of maternal closeness, living arrangements, race/ethnicity, and control variables to assess associations with depressive symptoms in adulthood (Wave V).
Findings
Summary Statistics
We describe weighted summary statistics of the analytic sample in Table 1. The majority of the sample is white (73%), with 14% being Black, 9% being Latinx, and 3% being Asian. The average respondent age at Wave V is about 38 years old. By Wave IV, the majority of respondents reported a close relationship with their mothers, with an average closeness of 4.52 on a scale from 1 to 5. A noticeable proportion of respondents (15%) live with their parents by Wave IV. By Wave V, respondents have somewhat low depressive symptoms, with an average score of 1.47.
Summary statistics
| Race and ethnicity | Mean | SE |
|---|---|---|
| Black | 0.14 | 0.02 |
| Latinx | 0.09 | 0.02 |
| Asian | 0.03 | 0.01 |
| white | 0.73 | 0.01 |
| Family structure (Wave I) | ||
| Two bio parents | 0.62 | 0.01 |
| Two parents | 0.16 | 0.01 |
| Single parent | 0.20 | 0.01 |
| Other | 0.02 | 0.00 |
| Gender | ||
| Female | 0.51 | 0.01 |
| Male | 0.49 | 0.01 |
| Immigrant generation status | ||
| 1st generation | 0.05 | 0.01 |
| 2nd+ generation | 0.95 | 0.01 |
| Age at Wave V | 37.69 | 0.10 |
| Maternal education (Wave I) | ||
| Did not graduate HS and less | 0.15 | 0.01 |
| HS graduate or GED | 0.37 | 0.01 |
| Some college | 0.21 | 0.01 |
| Completed college+ | 0.28 | 0.01 |
| Maternal closeness (Wave IV) | 4.52 | 0.01 |
| Live with parents (Wave IV) | 0.15 | 0.01 |
| Depression scale (CES-D at Wave V) | 1.47 | 0.01 |
| N | 8,970 |
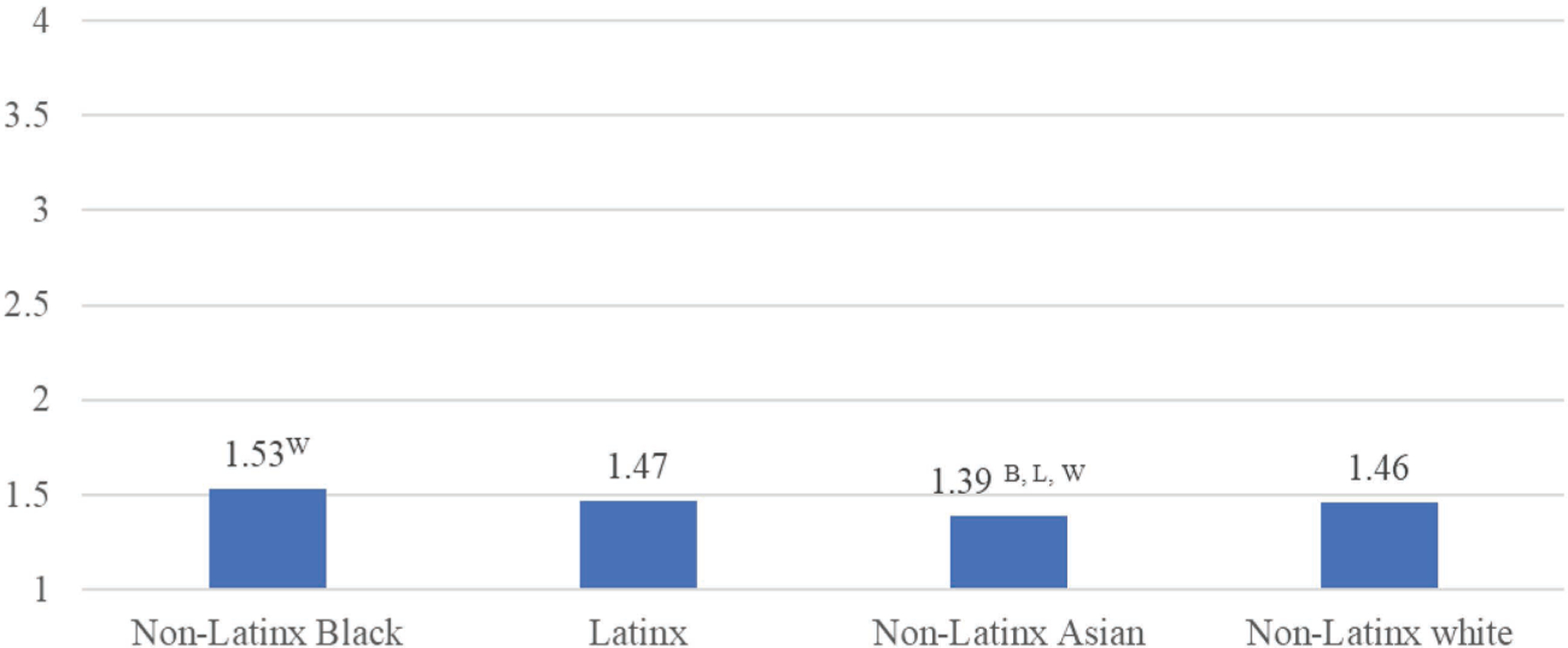
Mental Health across Race and Ethnicity
Figure 1 describes the differences in depressive symptoms in Wave V by respondents’ race/ethnicity. We find that Non-Latinx Black respondents have the highest reports of depressive symptoms, with an average score of 1.53. This average score is significantly different from non-Latinx white respondents, who have an average score of 1.46. Latinx respondents have an average depressive symptom score of 1.47, though this is not significantly different from any other group. Finally, we find that Asian respondents have the lowest depressive symptoms score of 1.39. This is significantly different from Black, Latinx, and white respondents.
Parent-Child Relationships and Mental Health across Race/Ethnicity
The results of our stepwise regressions predicting depressive symptoms at Wave V are described in Table 2. In Model 1, we estimate the following independent variables: respondents’ race and ethnicity, maternal closeness at Wave IV, and parent-child living arrangements at Wave IV. We find that all of these factors significantly predict respondents’ depressive symptoms. Respondents who identify as non-Latinx Black have significantly higher depressive symptoms compared to non-Latinx white respondents. Respondents who identify as non-Latinx Asian have significantly lower depressive symptoms. Respondents’ Latinx identity is not significantly associated with depressive symptoms when compared to non-Latinx white respondents. Maternal closeness significantly predicts lower depressive symptoms, while respondents’ living arrangement with their parents significantly predicts higher depressive symptoms, both at the p < 0.001 level.
OLS regressions predicting depressive symptoms at Wave V
| Model 1 | Model 2 | |
|---|---|---|
| Race and ethnicity (ref. group: non-Latinx white)—non-Latinx Black | 0.06** (0.02) |
0.03 (0.02) |
| Latinx | 0.00 (0.03) |
−0.04 (0.03) |
| non-Latinx Asian | −0.09** (0.03) |
−0.11** (0.03) |
| Maternal closeness at Wave IV | −0.07*** (0.01) |
−0.07*** (0.01) |
| Lived with parents at Wave IV | 0.12*** (0.02) |
0.12*** (0.02) |
| Gender: Female | 0.03* (0.01) |
|
| Family structure at Wave I (ref. group: two biological parents)—Two parents | 0.03 (0.02) |
|
| Single parent | 0.05* (0.02) |
|
| Other | 0.16* (0.07) |
|
| Immigrant generation status (ref. group: 2nd+ generation)— 1st generation | 0.02 (0.04) |
|
| Age at Wave V | 0.00 (0.00) |
|
| Maternal education at Wave I (ref. group: <High school degree)—High school degree | −0.06 (0.03) |
|
| Some college | −0.09** (0.03) |
|
| College+ | −0.08** (0.03) |
|
| 8970 | ||
| Exponentiated coefficients; Standard errors in parentheses |
-
p < 0.05;
-
p < 0.01;
-
p < 0.001
In Model 2, we include control variables to see if significant associations hold. We find that while the significant association between race and ethnicity and depressive symptoms disappears for non-Latinx Black respondents, non-Latinx Asian respondents continue to have significantly lower depressive symptoms than non-Latinx white respondents. Both maternal closeness and parent-child living arrangements remain significantly associated with respondents’ depressive symptoms at the p < 0.001 level. Multiple control variables are also significantly associated with respondents’ depressive symptoms at the p < 0.05 level. Additional control variables associated with increased depressive symptoms included respondents being assigned female at birth, respondents growing up in a single-parent family structure, and respondents growing up in some “other” family structure at Wave I. Maternal education is also significantly associated with depressive symptoms at the p < 0.01 level; respondents’ mother’s educational attainment of some college or college and beyond both predict lower depressive symptoms among young adults.
Specific Policy Recommendations
These results point to the complex interplay between race, ethnicity, parent-child relationships, and depressive symptoms in adulthood. Both maternal closeness and parent-child living arrangements continue to matter for respondents’ depressive symptoms, controlling for a host of covariates. These findings point toward the importance of the parent-child relationship in addressing and thinking about children’s depressive symptoms aging into adulthood. Policies focused on improving mental health should emphasize the importance of family and parental relationships more broadly and the ways these relationships may intersect with racial and ethnic identity.
Biographies
Dr. Xing Zhang’s research focuses on the role of parent-child relationships in shaping young adults’ health from adolescence to adulthood and how this varies across race, ethnicity, gender, and socioeconomic status.
Annaliese Grant’s research focuses on the classed dynamics of family relationships, responsibilities, and media use.
Notes
- Zhang, X., & Grant, A. (2021). Parent-child relationships and mental health in the transition to adulthood by race and ethnicity. Currents, (2)1.
References
Ackard, D. M., Neumark-Sztainer, D., Story, M., & Perry, C. (2006). Parent-child connectedness and behavioral and emotional health among adolescents. American Journal of Preventive Medicine, 30(1), 59–66. https://doi.org/10.1016/j.amepre.2005.09.013https://doi.org/10.1016/j.amepre.2005.09.013
Cooper, S. M., & McLoyd, V. C. (2011). Racial barrier socialization and the well-being of African American adolescents: The moderating role of mother-adolescent relationship quality. Journal of Research on Adolescence, 21(4), 895–903. https://doi.org/10.1111/j.1532-7795.2011.00749.xhttps://doi.org/10.1111/j.1532-7795.2011.00749.x
Davidson, T. M., & Cardemil, E. V. (2009). Parent-child communication and parental involvement in Latino adolescents. Journal of Early Adolescence, 29(1), 99–121. https://doi.org/10.1177/0272431608324480https://doi.org/10.1177/0272431608324480
Love, J. A., & Buriel, R. (2007). Language brokering, autonomy, parent-child bonding, biculturalism, and depression: A study of Mexican American adolescents from immigrant families. Hispanic Journal of Behavioral Sciences, 29(4), 472–491. https://doi.org/10.1177/0739986307307229https://doi.org/10.1177/0739986307307229
Moon, S. S., & Rao, U. (2010). Youth-family, youth-school relationship, and depression. Child and Adolescent Social Work Journal, 27(2), 115–131. https://doi.org/10.1007/s10560-010-0194-9https://doi.org/10.1007/s10560-010-0194-9
Morgan, Z., Brugha, T., Fryers, T., & Stewart-Brown, S. (2012). The effects of parent-child relationships on later life mental health status in two national birth cohorts. Social Psychiatry and Psychiatric Epidemiology, 47(11), 1707–1715. https://doi.org/10.1007/s00127-012-0481-1https://doi.org/10.1007/s00127-012-0481-1
Osborne, L. N., & Fincham, F. D. (1996). Marital conflict, parent-child relationships, and child adjustment: Does gender matter? Merrill-Palmer Quarterly, 42(1), 48–75.
Smith, D. E. (1993). The standard North American family: SNAF as an ideological code. Journal of Family Issues, 14(1), 50–65. https://doi.org/10.1177/0192513X93014001005https://doi.org/10.1177/0192513X93014001005
Smith, S. M., & Sun, R. (2014). Racial discrimination and depressive symptomology: Exploring gender and socioeconomic variations among African American parent-child dyads. Fire!!!, 3(1), 130–159. JSTOR. https://doi.org/10.5323/fire.3.1.0130https://doi.org/10.5323/fire.3.1.0130