Introduction
Afghanistan, officially the Islamic Emirate of Afghanistan, is a landlocked country located at the crossroads of central and south Asia. Referred to as the “Heart of Asia,” it is bordered by Pakistan, Iran, Turkmenistan, Uzbekistan, Tajikistan, and China. Afghanistan occupies 652,864 square kilometers (252,072 sq. mi.) of land. As of 2021, its population is 40.2 million, composed chiefly of ethnic Pashtuns, Tajiks, Hazaras, and Uzbeks. Afghanistan has the largest drug supply, opium production, and prevalence of opioid use disorder in the world (World Bank Report; Ward & Byrd, 2004). Herat province is the country’s largest city, and many of the population are involved with addiction, especially women deprived of medical and psychological treatment.
Substance use is a national epidemic that significantly burdens the health care system (Englander et al., 2017). The use of opium and other substances for medical and social purposes has been present in Afghanistan for centuries. In the last decade, intoxicant use has become more apparent, including opium, cannabis, and psychotropics such as prescription analgesics, benzodiazepine, and tranquilizers. Trends for substance use and patterns of risk behaviors further changed in the last years (Todd et al., 2012). UNODC (2010b) reported that injection use of opiates is rising in Afghanistan. Due to the rate of drug use and production, especially opium in Afghanistan, programs to reduce dependence on substance use have received less attention (Griffin & Khoshnood, 2010); also, research on Afghani women with SUD is scarce.
Substance Use Disorder is also associated with antisocial behavior, psychological disorders, and infectious diseases such as AIDS and hepatitis (Mozafarinia et al., 2017). Cottler et al. (2014) reported that overall substance use in individuals in Afghanistan was high, with a prevalence of 11% in men, 4% in women, and 2% in children. Opioids were the most common positive results. Opium use is most often found in the northeast and west regions and all provinces, with cannabinoids being the second most prevalent drug. Contrary to expectations, Cottler et al. (2014) did not find a high prevalence of prescription opioids in any region of Afghanistan. The low prevalence of polysubstance use among women (4%) and children (3%), compared with that of men (13%), was noteworthy. Moreover, 41% indicated that more women are using opium now than five years ago.
Epidemiological research and studies on psychiatric patients have documented the highest comorbid SUDs and mental health disorders (Andersson et al., 2019). A survey of SUD inpatients found that 40.5% of participants met the criteria for at least one comorbid Axis I disorder, with mood, anxiety, and somatoform disorders being reasonably common (Langenbach et al., 2010). Comorbidity of anxiety disorders and SUD is well-documented in the literature. In individuals with SUDs, anxiety disorder’s comorbidity is associated with greater clinical severity and poorer treatment outcomes, making it a severe public health concern (Wolitzky-Taylor et al., 2018).
Many studies have proposed the relationship between substance use or abuse and anxiety disorders in individuals who resort to these substances as a coping mechanism to tackle negative feelings. Some individuals may use substances in a controlled manner to alleviate the symptoms of anxiety. However, tobacco, alcohol, and other substance use are linked to weak medication effects and worsening psychiatric symptoms (De Matos et al., 2018). Chronic substance use can lead to a structural state of disinhibition over time, leading to chronic substance use. This state is observed in patients not exclusively in the acute stages of substance dependency but after stopping the regular substance use. Elevated levels of impulsivity are also associated with more severe symptoms of SUD, which eventually leads to higher levels of drug craving (Fielenbach et al., 2018). Craving is hypothesized to be one of the strongest and most consistent across diverse contexts and substances. Craving predicts substance use outcomes following treatment; a positive relationship exists between craving and the likelihood of substance use in the subsequent period (Enkema, & Bowen, 2017). Craving, a key concept in addiction, describes an urge or conscious desire to take a substance and is hypothesized to underlie substance seeking and relapse in substance users. Traditionally, craving is linked to brain areas related to reward, motivation, and memory, including the prefrontal cortical cortex, striatum, and ventral pallidum; as well as mesolimbic dopamine structures, such as the ventral tegmental area, and reward memory areas, such as the amygdala and the hippocampus (Moreno-Rius & Miquel, 2017).
Cox and Klinger (2004) assert that substance use results from the interaction between several elements, including biological and situational factors, substance use expectations, personality traits, and other psychological and socio-cultural factors. The result of the interaction between different factors in this model is the motivational structure. The motivational structure represents the goals and methods people pursue (Cox, Fadardi & Klinger, 2006). In this regard, the motivational structure can be considered a non-adaptive factor, diminishing the likelihood of employing successful solutions unrelated to the drug, thereby reinforcing motivation for emotional manipulation through chemical changes. In this model, the motivational structure is one of the main determinants of addictive behaviors (Cox, Fadardi & Klinger, 2006).
Over the past few years, various treatment programs have been introduced to treat Substance Use Disorders. Cognitive-Behavioral Therapy (CBT) is one of the psychotherapies that research has confirmed its efficacy in SUDs (McHugh et al., 2010). However, it should be noted that Cognitive-Behavioral Therapy has its limitations. For example, while it determines irrational beliefs are significant causes of Substance Use Disorder, the CBT effects appear over time and decrease during a nine-month follow-up (Magill and Ray, 2009).
It has been argued that a possible reason for CBT’s lack of efficacy might be due to residual symptoms and mechanisms at a metacognitive level. The main focus of CBT is modifying the content of biased cognitive beliefs. However, it does not directly modify the driver of maladaptive cognitive processes called metacognitive beliefs (Caselli et al.,2018). Moreover, researchers have found direct or indirect relations between meta-cognition and drinking problems (Spada & Wells, 2009) and drug dependency (Toneatto, 1999).
MCT is theoretically derived from the self-regulatory executive function (S-REF) model. The S-REF model argues that Cognitive Attentional Syndrome (CAS) is a perseverative thinking style that causes psychopathology. The CAS consists of dysfunctional coping strategies that individuals adopt to manage distressing thoughts and feelings. In MCT, metacognitive beliefs and processes related to CAS were identified and modified during treatment. The patients were instructed to postpone their concerns and rumination. Overall, MCT seeks to boost the experience of attentional control in individuals, reduce self-focused attention, and foster the development of adaptive beliefs and coping strategies (Wells, 2011; Normann & Morina, 2018). A significant component of CAS is perseverative negative thinking in the form of rumination or worry. Rumination or worry is linked to particular metacognitive beliefs and processes (Papageorgiou & Wells, 2003). The metacognitive beliefs behind the CAS are conceptualized as positive beliefs concerning the use of disturbing, negative thoughts that emphasize the uncontrollability and harmfulness of one’s worries (Capobianco et al., 2020). Spada and Wells (2008) found that positive and negative metacognitive beliefs predict alcohol use and drinking problems irrespective of their negative emotions in community and clinical samples. The relation between metacognitive beliefs and alcohol use and the development and persistence of emotional dysfunction is essential. Positive and negative metacognitions drive individuals to start and perpetuate alcohol use as a cognitive-emotional regulatory strategy (Ottonello et al., 2019).
Many studies reported the effectiveness of MCT (Ost, 2008; Normann & Morina, 2018; Caselli et al., 2018). However, the severity of the disorder determines the effects of SUD on a specific family; other serious factors include psychiatric illness, the behaviors of a family member with SUD, family support, and the family members coping strategies. Under these conditions, family members may feel helpless, hopeless, betrayed, ashamed, worried, angry, depressed, anxious, and demoralized. In addition, families may endure high rates of tension and conflict related to SUD, leading to family breakup due to separation and divorce (Daley, 2013; Delay et al., 2018).
So, MCT is one of the most critical interventions that focus on the individual’s negative and dysfunctional thoughts and feelings, improving a substance users’ mental health by trying to change the content of negative thoughts, beliefs, and emotions. Working on negative thoughts and challenging them, which play an essential role in perpetuating addiction, becomes a driving force that positively affects the psychological health of substance users and paves the way for them to improve.
There is evidence that some psychotherapies are inconsistent with Islamic beliefs and unsuitable for Muslim clients (Abu Raiya & Pargament, 2010). Also, researchers argue that contemporary psychotherapies may not be appropriate for minority groups such as Muslims (Koç & Kafa, 2019). However, it seems that the MCT content and procedures are congruent with Islamic teachings, and MCT may be an appropriate psychotherapy for Muslim patients.
Methods
This study was conducted using a randomized open-labeled controlled clinical trial. The study population was Muslim women with Substance Use Disorder referred to state addiction clinics by physicians from health centers in Herat. In 2021, 30 Muslim women with an SUD were selected using the available and targeted sampling method.
The researchers randomly divided the participants into two groups (N = 15 in the MCT group and N = 15 in the waiting list). The participants on the waiting list received methadone maintenance therapy, whereas the experimental group received MCT (Saulsman, Anderson, Campbell & Swan & Sng, 2017). The treatment lasted 45 days, and the participants completed the research questionnaires in three stages: pre-test, post-test, and follow-up (after 60 days). Inclusion criteria included the following: history of substance use (use of opium or other drugs for at least one year), 25–35 years of age, signed informed consent form, willingness to participate in the study, and minimum reading literacy.
The exclusion criteria included missing more than three treatment sessions, acute psychiatric illness, and a history of substance use for less than one year.
Most participants were between 25–30 years old (66.7% in the MCT group and 53.3% in the control group). The two groups were not significantly different in age (p = 0.45). Most participants had primary education in the MCT group or were illiterate (33.3%), and in the control group, most subjects had high school diplomas or were illiterate (33.3%). The two groups were not significantly different in level of education (p = 0.25). In the MCT group, seven subjects were single (46.7%) and eight were married (53.3%), and in the control group, four subjects were single (26%), and eleven were married (73.3%). The two groups were not significantly different in marital status (p = 0.25). In the experimental group, 46.7% had no children, 26.7% had four children, and 13.3% had two or three children. In the TAU group, 33.3% had two children, 26.7% had no children, 20% had four children, and 6.7% had one, three, or five children.
Materials
Regarding the validity and reliability of the questionnaire, due to cultural, religious, and linguistic similarities between Iran and Afghanistan, and the fact that the questionnaires were applied in the same original language, the Iranian psychometric properties of the questionnaires were assumed to be similar.
Demographic Information
Participants’ demographic information, including age, education, and marital status, was obtained using a researcher-made questionnaire after completing an informed consent form.
The Metacognitive Questionnaire (MCQ-30)
The questionnaire, developed by Wells & Cartwright Hatton in 2004, is a 30-item self-report instrument that assesses individuals’ metacognitive beliefs. The items are scored on a 4-point Likert scale from 1 (strongly disagree) to 4 (strongly agree). This questionnaire comprises five subscales: positive beliefs, negative beliefs about uncontrollability and danger of thoughts, cognitive trust, beliefs about the necessity of controlling thoughts, and cognitive self-awareness. Higher scores indicate higher levels of maladaptive, metacognitive beliefs. The MCQ-30 had good internal consistency, convergent validity, and acceptable test-retest reliability (Spada, Mohiyeddini & Wells, 2008; Wells & Cartwright-Hatton, 2004). Wells & Cartwright-Hatton (2004) reported internal consistency for the whole scale as 0.93 and for the subscales, respectively, 0.93, 0.92, 0.92, 0.91, and 0.72. Shirinzadeh et al. (2009) assessed the psychometrics of Iranian MCQ-30. They reported the Cronbach’s alpha as 0.91 for the whole scale, and the individual subscales ranged 0.71–0.87. Test-retest reliability coefficients after a 4-week interval was reported as 0.73 for the total score, and subscales ranged 0.59–0.83.
Beck Anxiety Inventory (BAI)
Beck et al. (1988) introduced the Beck Anxiety Inventory (BAI), which measures individuals’ clinical anxiety symptoms. The BAI is a 21-item questionnaire with a 4-point scale ranging from 0 (not at all) to 3 (severely). The total score of the questionnaire ranged 0–63. The instrument has excellent internal consistency (0.92), and the test-retest reliability by a one-week interval was appropriate (r=0.75) (Beck & Steer, 1990). In the Iranian sample, BAI showed desirable validity and reliability (Kaviani & Mousavi, 2008).
Beck Depression Inventory-II (BDI-II; Beck & Steer, 1996)
This inventory is the revised form of the Beck Depression Inventory designed to assess the severity of depressive symptomatology. This 21-item inventory is scored on a scale of 0–3. The cut-off points are as follows: slight depression (0–13), mild depression (14–19), moderate depression (20–28), and severe depression (29–63). Typically, the scores of the clinically depressed individuals are from 12–40. Wang & Gorenstein (2013) reported internal consistency of around 0.9, and the test-retest reliability ranged 0.73–0.96. This study used the Persian version of the BDI-II, which had appropriated psychometric properties (Mohammadkhani & Massah-Choulabi, 2007). Mohammadkhani & Massah-Choulabi (2007) reported the Persian BDI-II’s Cronbach’s alpha coefficient as 0.92 for outpatients and 0.93 for students. The reliability coefficient was approved by the test-retest method (0.93). The BDI-II’s construct and factor validity has also been confirmed (Mohammadkhani & Massah-Choulabi, 2007).
Substance Use Evaluation Questionnaire
This questionnaire was developed by Fadardi, Ziaee, & Bar Erfan (2008). This Likert-based scale contains 20 items that measure thoughts and fantasies related to substance, substance use, and withdrawal. Each item is scored on a graded scale from 0 (entirely true) to 5 (completely wrong), and its total score ranges 0–100. The reliability of this questionnaire was measured using internal consistency, and a Cronbach alpha of 0.94 was reported. Fadardi, Bar Arfan, & Amin Yazdi (2010) also approved the convergent validity of the scale using the situational confidence questionnaire (Annis and Graham,1998).
The Personal Concern Inventory (PCI)
The PCI is the revised and abridged version of the Motivational Structure Questionnaire (MSQ) and was developed by Cox, Klinger, and Fadardi (2006). The PCI measures motivational structure. This questionnaire expresses the personal concerns of the subjects in different areas of life and their goals for resolving problems related to each concern. They also rated their goal-seeking in various dimensions, such as expected chances of success or the necessary information about the goal, reflecting their motivational structure. Subjects score items on an eleven-point Likert score from 0–10. According to rank scales, adaptive motivational scores can be calculated. Fadardi (2003) assessed the reliability of the questionnaire using Cronbach’s alpha for the sample of students (r = 0.77) and alcohol users (r = 0.75).
Situational Confidence Questionnaire
This 16-item questionnaire, developed by Annis and Graham (1998), measures self-efficacy in different substance use situations, including favorable situations, social issues at the workplace, social tension, physical discomfort, and a self-control test in which subjects are asked to imagine themselves in different situations and evaluate their resistance to drug-abuse craving.
The items of this questionnaire are divided into eight subscales and scored on the Likert scale ranging from 0 (completely uncertain) to 100 (entirely sure). The overall score of this questionnaire is usually considered. The questionnaire’s internal consistency reliability was assessed on 536 substance users, and a Cronbach’s alpha of 0.93 was reported (Fadardi & Ziaee, 2009).
Procedure
In this study, due to war conditions in Afghanistan, a voluntary sampling method was used, and 30 Muslim women with Substance Use Disorder that were referred to women’s addiction treatment clinics in Herat were selected. They were randomly divided into experimental and control (waiting list) groups. Both groups completed the questionnaires at the baseline. The women referred to the clinics voluntarily used opium, heroin, cannabis, and heroin products. The MCQ, BAI, Beck Depression Inventory (BDI-II), Substance Use Evaluation Questionnaire, Personal Concern Inventory, and Situational Confidence Questionnaire were applied to obtain the baseline scores of participants in the experimental and control groups. The experimental group attended six sessions of 90-min MCT. All the therapists were women, lived in Herat, Afghanistan, and had a master’s degree in psychology or counseling. The control group received the addiction clinic’s routine treatment.
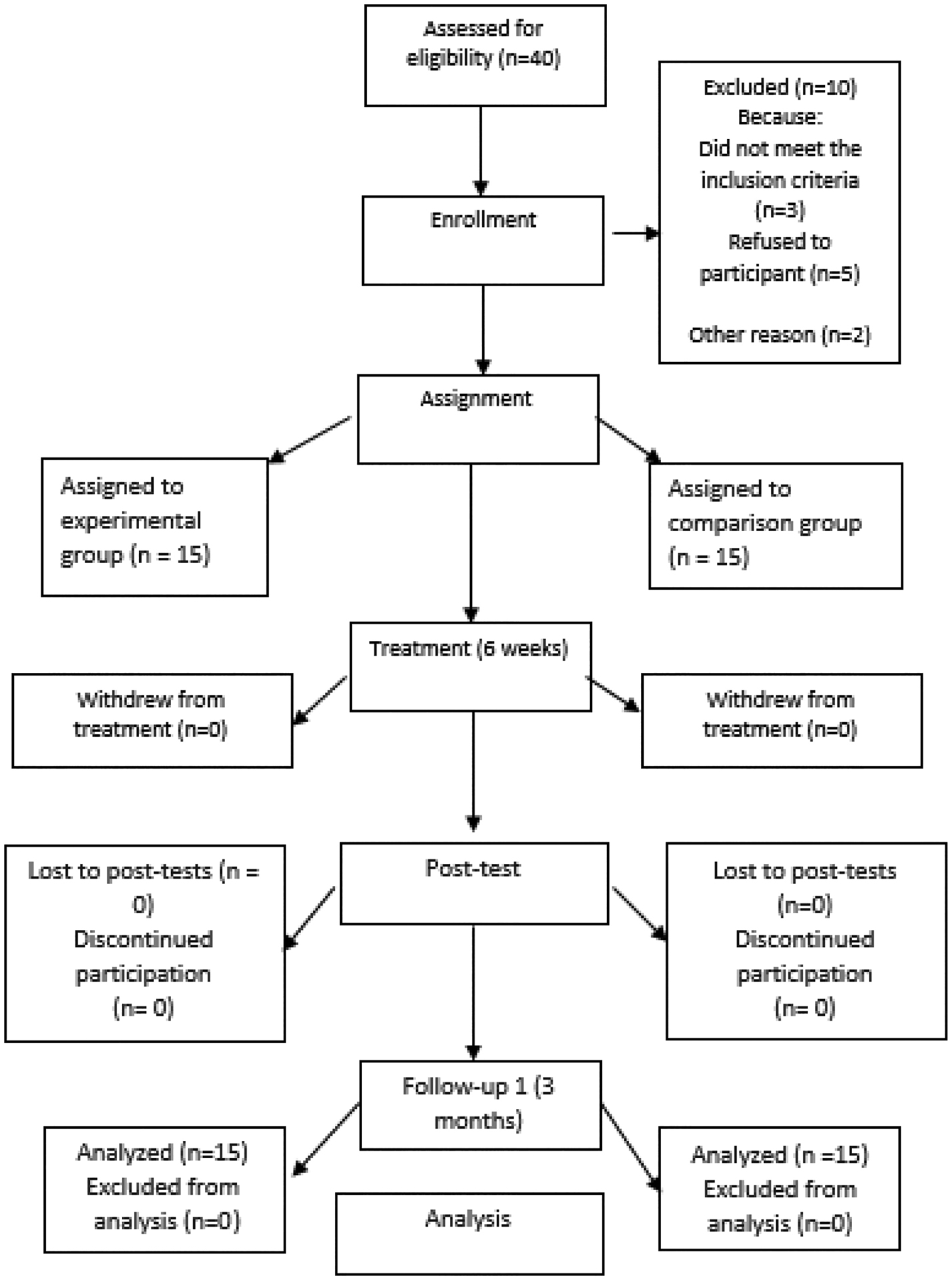
Acute psychological disorders were assessed by a psychiatrist through a Structured Clinical Interview for DSM-5 at an addiction clinic, and people with acute psychiatric disorders were excluded from treatment. Women absent for more than three sessions were excluded from treatment and continued the methadone treatment only. For women who could not complete the questionnaires and were poorly literate, the researcher read the questions to them and recorded their answers on a piece of paper. Also, we tried to prevent dropping out by using a consent form and managing the clients’ limitations before session entry. The participants filled out questionnaires at the end of the MCT sessions in the experimental group and the Treatment as Usual (TAU) programs in the control group (Methadone Maintenance Therapy), which lasted 45 days. They once again completed the questionnaires after a three-month follow-up. Figure 1 shows the participants’ flow in this study. A summary of the MCT protocol derived from the Saulsman et al. (2017) protocols are presented in Table 1.
The Main topics Covered in the MCT Sessions
Sessions |
Content |
|---|---|
First |
Establishing a therapeutic relationship, setting group rules, explaining the structure of meetings and the importance of tasks, introducing members to each other, explaining what they know about worry and rumination, defining the concepts of worry and rumination, explaining factors of worry and rumination, identifying protective factors, and presenting the task of monitoring rumination and worry |
Second |
Reviewing the task of the previous session, challenging the remaining uncontrollable metacognitions, setting the behavioral test of procrastination, training attention and its practice in the session, practicing procrastination and attention as the session's task |
Third |
Training attention, reviewing tasks of the previous session, challenging the remaining uncontrollable metacognitions, challenging dangerous metacognitions, setting up behavioral tests for dangerous beliefs, and doing exercises to challenge rumination for the next session |
Fourth |
Practicing attention in the session, reviewing the previous session's task, and challenging the remaining negative metacognitions, challenging the positive metacognitions, setting the behavioral test, exploring the ups and downs of worry, and presenting behavioral testing and attention training as homework for the next session to practice |
Fifth |
Practicing mindfulness in the session, reviewing the task of the previous session, changing metacognition and metacognitive beliefs that remain positive, challenging ineffective behaviors, and adopting active coping strategies, and assigning the task of mindfulness and active coping strategy for the next session |
Sixth |
“Abandoning” exercise, reviewing previous session assignments, reviewing treatment progress and self-management planning, reviewing general principles of MCT, reviewing progress, and preparing for the future |
Results
The present study was performed on 30 women with Substance Use Disorder (N = 15 in the experimental group and N = 15 in the control group).
Table 2 shows the descriptive indicators of metacognitive beliefs, situation-dependent confidence, adaptive motivation, withdrawal craving assessment, anxiety, and depression in the pre-test, post-test, and follow-up stages for the experimental and control groups. Table 2 shows that the interaction effects of time and group on positive beliefs about worry (F (2,56) = 37.11, p < 0.001), negative beliefs about uncontrollability and dangerous thoughts (F (2,56) = 33.63, p < 0.001), cognitive trust (F (2,56) = 62.23, p < 0.001), beliefs about the need to control thoughts (F (2,56) = 73.50, p < 0.001), cognitive self-awareness (F (2,56) = 29.42, P < 0.001), Situational Confidence Questionnaire (F(1.61, 45.08) = 66.20, p < 0.001), Personal Concern Inventory (F (1.22, 34.36) = 5.45, p < 0.001), Substance Use Evaluation (F (1.57, 44.02) = 6.12, p < 0.001), anxiety (F (2,56) = 14.48, p < 0.001), and depression (F (2,56) = 42.47, p < 0.001) were also significant. This result suggests a significant difference between the experimental and control groups in diminished situation-dependent confidence, adaptive motivation, withdrawal craving, anxiety, and depression from the pre-test to the follow-up.
Comparison of variables at pre-test, post-test, and follow-up phases in the MCGT and TAU groups
Variables |
Pre-test (mean ± SD) |
Post-test (mean ± SD) |
Follow-up (mean ± SD) |
Repeated measure ANOVA |
|||
|---|---|---|---|---|---|---|---|
Time |
Time*group |
P |
|||||
MCQ (Total score) |
MCT |
93.20 ± 5.21 |
59.20 ± 8.92 |
54.53 ± 6.28 |
F(1.46,40.99) = 29.60 |
F (1.46,40.99) = 86.81 |
0.001 |
Control |
80.20 ± 8.35 |
89.06 ± 10.29 |
90.40 ± 4.28 |
||||
Positive beliefs about worry |
MCT |
17 ± 1.77 |
11.60 ± 1.91 |
11.40 ± 2.06 |
F(2,56) = 14.82 |
F (2,56) = 37.11 |
0.001 |
Control |
16.80 ± 2.36 |
18.33 ± 1.29 |
17.80 ± 1.52 |
||||
Negative beliefs about the uncontrollability and danger of worry |
MCT |
17.86 ± 1.06 |
11.73 ± 2.05 |
10 ± 1.51 |
F (2,56) = 13.98 |
F (2,56) = 33.63 |
0.001 |
Control |
16.33 ± 2.89 |
17.06 ± 2.65 |
18.33 ± 1.95 |
||||
cognitive trust |
MCT |
18.86 ± 1.68 |
11.60 ± 1.88 |
10.46 ± 2.26 |
F(2,56) = 16.51 |
F(2,56) = 62.23 |
0.001 |
Control |
14.80 ± 2.27 |
17.26 ± 2.49 |
17.40 ± 1.63 |
||||
beliefs about the need to control thoughts |
MCT |
17.33 ± 1.38 |
11.13 ± 1.92 |
10.20 ± 1.85 |
F(2,56) = 12.19 |
F(2,56) = 73.50 |
0.001 |
Control |
14.26 ± 2.28 |
17.33 ± 2.60 |
17.26 ± 1.98 |
||||
cognitive self-awareness |
MCT |
21.73 ± 2.60 |
13.13 ± 2.64 |
12.46 ± 2.47 |
F(2,56) = 15.96 |
F(2,56) = 29.42 |
0.001 |
Control |
18 ± 4.03 |
19.06 ± 2.98 |
16.60 ± 2.41 |
||||
SCQ (Total score) |
MCT |
308 ± 63.60 |
782.66 ± 107.66 |
862 ± 122.89 |
F(1.61,45.08) = 136.13 |
F(1.61,45.08) = 66.20 |
0.001 |
Control |
312.26 ± 53.78 |
372 ± 139.14 |
428 ± 154.32 |
||||
PCI (Total score) |
MCT |
323.73 ± 37.96 |
460.46 ± 25.80 |
480 ± 20.67 |
F(1.22,34.36) = 7.68 |
F(1.22,34.36) = 5.45 |
0.001 |
Control |
410.33 ± 41.17 |
426.40 ± 12.97 |
423 ± 28.95 |
||||
substance Use Evaluation Questionnaire (Total Score) |
MCT |
79.26 ± 2.71 |
71.13 ± 6.15 |
67.60 ± 4.33 |
F (1.57,44.02) = 20.68 |
F (1.57,44.02) = 6.12 |
0.001 |
Control |
86.53 ± 5.26 |
83.46 ± 4.37 |
83.26 ± 5.82 |
||||
BAI |
MCT |
40 ± 6.60 |
23.20 ± 9.95 |
19.66 ± 9.20 |
F (2,56) = 37.45 |
F (2,56) = 14.48 |
0.001 |
Control |
46.93 ± 4.35 |
43 ± 8.12 |
42.20 ± 7.62 |
||||
BDI-II |
MCT |
47.86 ± 5.37 |
23.46 ± 8.28 |
18.20 ± 5.42 |
F (2,56) = 164.10 |
F (2,56) = 42.47 |
0.001 |
Control |
42.20 ± 7.62 |
43.20 ± 6.34 |
38.20 ± 7.37 |
||||
*Results of the repeated measured Analysis of variance within subjects
Note.
The results of Table 3 show that the independent variable (MCT group) had a significant effect on the subscales of metacognitive beliefs, situation-dependent confidence, adaptive motivation, withdrawal craving, anxiety, and depression in the experimental group. In addition, the MCT group influenced the subscales of metacognitive beliefs, situation-dependent confidence, adaptive motivation, withdrawal craving, anxiety, and depression.
Repeated Measured Analysis of Variance Between Participants
Variables |
Group |
F |
p |
Effect size |
|---|---|---|---|---|
MCQ (Total score) |
Intervention |
Time: F (1,28) =55.87 |
0.001 |
0.66 |
Control |
Time*group= F (1,28) = 164.64 |
0.001 |
0.85 |
|
Positive worry beliefs |
Intervention |
Time: F (1,28) = 17.994 |
0.001 |
0.39 |
Control |
Time*group= F (1,28) = 36.94 |
0.001 |
0.56 |
|
Beliefs about uncontrollability and danger of worry |
Intervention |
Time: F (1,28) = 21.52 |
0.004 |
0.43 |
Control |
Time*group= F (1,28) = 60.89 |
0.001 |
0.68 |
|
Meta-cognitive efficiency |
Intervention |
Time: F (1,28) = 34.76 |
0.001 |
0.55 |
Control |
Time*group= F (1,28) = 125.04 |
0.001 |
0.81 |
|
General negative beliefs |
Intervention |
Time: F (1,28) = 24.55 |
0.001 |
0.46 |
Control |
Time*group= F (1,28) = 132.58 |
0.001 |
0.82 |
|
Cognitive self-consciousness |
Intervention |
Time: F (1,28) = 20.98 |
0.001 |
0.42 |
Control |
Time*group= F (1,28) = 42.13 |
0.001 |
0.60 |
|
SCQ |
Intervention |
Time: F (1,28) = 169.11 |
0.001 |
0.85 |
Control |
Time*group= F (1,28) = 72.63 |
0.001 |
0.72 |
|
PCI |
Intervention |
Time: F (1,28) = 73.56 |
0.001 |
0.72 |
Control |
Time*group= F (1,28) = 35.15 |
0.001 |
0.62 |
|
Drug Use Evaluation Questionnaire |
Intervention |
Time: F (1,28) = 27.51 |
0.001 |
0.49 |
Control |
Time*group= F (1,28) = 8.70 |
0.68 |
0.23 |
|
BAI |
Intervention |
Time: F (1,28) = 51.78 |
0.001 |
0.64 |
Control |
Time*group= F (1,28) = 20.05 |
0.001 |
0.41 |
|
BDI-II |
Intervention |
Time: F (1,28) = 275.54 |
0.001 |
0.90 |
Control |
Time*group= F (1,28) = 58.66 |
0.001 |
0.67 |
*Results of the repeated measured analysis of variance between participants
Note:
Discussion and Conclusion
This study evaluated the effectiveness of MCT in improving psychological symptoms. According to the results, Metacognitive Therapy was effective in reducing depressive symptoms. This finding is aligned with the results reported in the literature, including Yaghobi et al. (2013), Wells et al. (2012), Ashoori (2015), Norman, Van Emmerik, & Morina (2014), and Hagen et al. (2017).
In explaining these findings, it can be argued that one of the critical factors contributing to depression is rumination, especially in people with substance use. This treatment enabled the patient to break the mental rumination about substance use, inhibit useless self-monitoring tendencies, and develop adaptive styles. The goal was to promote flexible metacognitive control and awareness in the patient and prevent mental processing in worry and rumination (Wells & Sembi, 2004). The MCT focuses on rumination and positive and negative metacognitions about substance use. Rumination and metacognitions of substance use declined following the mindfulness techniques introduced in the session, which led to a subsequent improvement in depression. The emotional vulnerability’s metacognitive model refers to the functions and consequences of perseverative negative thinking (such as depressive rumination and anxious worry). Ruminative thinking can be symptomatic of depression (Papageorgiou & Wells, 2001). Based on this model, depression is maintained and intensified by activating rumination and maladaptive response patterns (Wells, 2011). From a therapeutic perspective, modifications of positive and negative beliefs about worry or rumination are beneficial to treating emotional disorders (Papageorgiou & Wells, 2001).
The therapist explicated that whenever the subjects experience disturbing thoughts or symptoms of substance use, they should be alert and conscious of this situation, remind themselves not to worry about substance use, and only wait for the symptoms to disappear. The therapist asked clients to use mindfulness and procrastination to respond to all disturbing thoughts associated with substance use. MCT can reduce the anxiety of women with substance use. This finding was in line with those reported by Bergersen et al. (2011), Barnhofer et al. (2009), Wells et al. (2012), and Lakshmi et al. (2016). In addition, MCT stressed positive and negative metacognitive beliefs about substance use and reduced anxiety. According to the meta-cognitive theory, a triggering factor of anxiety was activating positive and negative metacognitive beliefs. This model underlines strategies that lead patients to modify and neutralize these triggering factors to control their anxiety (Ashoori et al., 2014).
Also, women with substance use deal with negative beliefs about worry, undermining their ability to control such thoughts and doubt their capabilities. As a result, they feel less self-confident, assuming they are not strong enough to resist drug cravings. The person finds themselves at an impasse in this situation and concludes that worry and anxiety help with handling the situation.
The metacognitive model asserted that individuals with anxiety hold positive beliefs about worrying as an effective means of dealing with that threat (Wells, 2006). In MCT, shifting attention from disturbing stimuli to other stimuli and their procrastination reduces anxiety in the individual. The subjects’ metacognitive beliefs about the uncontrollability of anxiety and worry were challenged and amended. Because of the fusion of thought, individuals need to take their thoughts and concerns seriously and be cautious about their frequency (Hazlett-Stevens, Zucker & Craske, 2002). As a result, coping techniques with thought-fusion metacognitions about substance use also helped them mitigate their anxiety. Additionally, teaching relaxation techniques such as mindfulness helped individuals to cope with anxiety.
Another finding of the study was that MCT was effective in improving metacognitive beliefs. The focus of MCT was on negative beliefs and thoughts as the consequences of controlling metacognitive beliefs and how such beliefs affect the continuity and change of cognition. MCT changed positive and negative metacognitive beliefs about substance use. In this approach, disturbing thoughts and dysfunctional beliefs were not challenged. However, they were linked to thoughts related to substance use in a way that prevents resistance or complex perceptual analysis, thereby overcoming dissenting thinking strategies about substance use. Thus, the MCT challenged the thought fusion. On the other hand, participants learned how to develop a more open metacognitive approach and process information that did not inefficiently stimulate the performance of the executive performance model. The technique of distancing and mindfulness achieved this goal.
Another finding of the study was that MCT could promote situational confidence. A situational confidence questionnaire measures how confident a person is about their ability to resist the urge or craving for substance use in certain situations, which is typical for different substance users worldwide. MCT helped individuals with substance use disorder develop a sense of self-integrity and self-confidence to behave effectively under specific circumstances.
The results also showed that substance craving and adaptive motivation improved subjects from pre-test to follow-up. This data is aligned with the findings reported by Mokhtari, Hassanzadeh, & Mirzaeeyan (2019); Caselli et al. (2018); and Spada, Caselli, & Wells (2013).
People with Substance Use Disorder hold strong craving ideas and beliefs about rumination suppression. In MCT, working on rumination and metacognition about substance use helped individuals improve their self-efficacy. Dysfunctional beliefs about substance use persuade them to seek substance, leading to substance use continuity as inappropriate coping behavior. During substance use, metacognitions are disrupted, coping skills are undermined by impaired metacognition, irrational beliefs and maladaptive behaviors are formed, and the ground is prepared for substance use (Abolghasemi et al., 2010). In MCT, metacognitive beliefs that lead to the formation of craving ideas and substance-related beliefs are challenged and modified, and maladaptive coping behaviors of substance use are prevented. Mindfulness and attention diversion techniques effectively diminished temptation and the likelihood of recurrence. The mindfulness technique diverted attention away from substance-related symptoms, resulting in people’s diminished temptation for substance use.
Substance users suffer from high cognitive distortions and dysfunctional thoughts. Studies showed that addiction is influenced by beliefs and attitudes (Holman, 2004; Skinner & Aubin, 2010). Substance use disrupts the cognitive system and creates a repetitive thinking style in the form of worry and rumination focused on the threat, little attention, and the adoption of mind control strategies (such as thoughts suppression). These factors resulted in cognitive symptoms and maladaptive behaviors (such as avoidance and substance use) (Wells, 2011).
In MCT, dysfunctional thought patterns about substance use were identified and modified, and individuals were empowered. Moreover, metacognitions were challenged using mindfulness and control techniques, mental rumination was disrupted, and disturbing regulatory tendencies declined. The concentration and attention of the addicted individuals were enhanced, leading to a change in their dysfunctional attitudes. The treatment focused on discarding disturbing thoughts and ruminations about substance use and avoiding catastrophizing events, which was obtained through illustrations and allegories. Such mechanisms could underlie clinical metacognitive efficacy, including diminished self-focused attention, the disruption of thought processing strategies driven by concerns and rumination about substance use, upgraded executive control on thought processing and attention, and reinforced metacognitive processing methods.
Conclusion
The present study showed that MCT could improve users’ psychological symptoms and be a therapeutic approach for Muslim women with substance use. This treatment significantly affects depression, anxiety, situational confidence, substance use, and personal concerns. This change indicates the treatment’s success in all experimental group members from pre-test to follow-up. Given the effectiveness of this treatment, it can offer a new approach to facilitating change and behavior that could be widely used in addiction interventions. MCT has been successful, and patients have exhibited no signs of exacerbation in depression, anxiety, or cravings.
This research had some limitations. Lack of controlled conditions for more accurate monitoring of tasks at home, short follow-up periods, the sample restriction to two addiction treatment clinics in Herat city, and use of self-report tools were some of the project’s limitations.
While attempting to overcome these limitations, it is suggested that a follow-up phase exceeding three months should be considered. It is also recommended to perform MCT individually to achieve more accurate training results. On the other hand, the effectiveness of MCT should be examined on other substance users, such as alcoholics and smokers, according to variables such as type, method, and duration of consumption. Also, MCT should be compared to methadone maintenance therapy used as a conventional treatment for SUD. This study focused on Afghani women who were using opium, so it is recommended to evaluate the effectiveness of other psychotherapies on them and repeat such studies on men. Additionally, due to cultural differences between Afghanistan as a Muslim country and the Western countries, where MCT and other types of modern psychotherapies were born, it is necessary to investigate the effectiveness of modern psychotherapies for the Muslim population. Finally, the study could have been enhanced by looking at drug use outcomes and satisfaction.
Further research is also warranted to develop a treatment model to identify risk factors for substance use and effective treatment to reduce psychological problems in substance users.
Data Transparency Disclosure
We have not previously published, nor do we currently have works in press stemming from this data set. All the research materials and data files are available.
Acknowledgment
We thank the participants who attended the psychotherapeutic sessions and carefully answered the research scales.
Declaration of Conflicts of Interest
The authors have no conflict of interest to disclose and received no research fund. The APA Ethical codes were approved in this research. Research Ethics committees of the Ferdowsi University of Mashhad declared that this project follows the ethical principles, national norms, and standards for conducting medical research in Iran (Approval ID: IR.UM.REC.1400.176).
References
Abolghasemi, A., Golpoor, R., Narimani, M., & Ghamari, H. (2010). The Relationship of Destruction Meta-Cognition Beliefs with Academic Achievement of Students with Test Anxiety. Research in Clinical Psychology and Counseling, 10(3),5–20. DOI: 10.22067/IJAP.V10I3.694310.22067/IJAP.V10I3.6943
Ashoori, J. (2015). Comparing the Effectiveness of Meta-Cognitive Therapy and Schema Therapy on Decrease Symptoms of Anxiety and Depression in Nursing and Midwifery Students. Journal of Arak University of Medical Sciences, 18(2), 50–61.
Abu Raiya, H., & Pargament, K. I. (2010). Religiously integrated psychotherapy with Muslim clients: From research to practice. Professional Psychology: Research and Practice, 41(2), 181–188. https://doi.org/10.1037/a0017988https://doi.org/10.1037/a0017988
Andersson, H. W., Lilleeng, S. E., Ruud, T., & Ose, S. O. (2020). Substance use among patients in specialized mental health services in Norway: prevalence and patient characteristics based on a national census. Nordic Journal of Psychiatry, 75 (3),160–169. https://doi.org/10.1080/08039488.2020.1817553.https://doi.org/10.1080/08039488.2020.1817553
Barnhofer, T., Crane, C., Hargus, E., Amarasinghe, M., Winder, R., & Williams, J. M. G. (2009). Mindfulness-based cognitive therapy as a treatment for chronic depression: A preliminary study. Behavior research and therapy, 47(5), 366–373. https://doi.org/10.1016/j.brat.2009.01.019.https://doi.org/10.1016/j.brat.2009.01.019
Bergersen, H., Frøslie, K. F., Sunnerhagen, K. S., & Schanke, A. K. (2010). Anxiety, depression, and psychological well-being 2 to 5 years poststroke. Journal of stroke and Cerebrovascular diseases, 19(5), 364–369. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.06.005https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.06.005
Beck, A. T., & Steer, R. A. (1990). Manual for the Beck Anxiety Inventory. San Antonio, TX: Psychological Corporation.
Caselli, G., Martino, F., Spada, M. M., & Wells, A. (2018). Metacognitive therapy for alcohol use disorder: A systematic case series. Frontiers in Psychology, 9, 2619. https://doi.org/10.3389/fpsyg.2018.02619https://doi.org/10.3389/fpsyg.2018.02619
Capobianco, L., Faija, C., Husain, Z., & Wells, A. (2020). Metacognitive beliefs and their relationship with anxiety and depression in physical illnesses: A systematic review. PloS one, 15(9), e0238457. https://doi.org/10.1371/journal.pone.0238457https://doi.org/10.1371/journal.pone.0238457
Cox, W. M., & Klinger, E. (2004). A motivational model of alcohol use: Determinants of use and change. In W. M. Cox & E. Klinger (Eds.), Handbook of motivational counseling: Concepts, approaches, and assessment (pp. 121–138). Chichester, England: Wiley. https://doi.org/10.1037//0021-843x.97.2.168https://doi.org/10.1037//0021-843x.97.2.168
Cox, W. M., Klinger, E., & Fadardi, J. S. (2015). The motivational basis of cognitive determinants of addictive behaviors. Addictive Behaviors, 44, 16–22. https://doi.org/10.1016/j.addbeh.2014.11.019https://doi.org/10.1016/j.addbeh.2014.11.019
Cox, W. M., Fadardi, J. S., & Klinger, E. (2006). Motivational Processes Underlying Implicit Cognition in Addiction. In R. W. Wiers & A. W. Stacy (Eds.), Handbook of implicit cognition and addiction (pp. 253–266). Sage Publications, Inc. https://doi.org/10.4135/9781412976237.n1713.https://doi.org/10.4135/9781412976237.n1713
Caselli, G., Martino, F., Spada, M. M., & Wells, A. (2018). Metacognitive therapy for alcohol use disorder: A systematic case series. Frontiers in Psychology, 9, 2619.
Cottler, L. B., Ajinkya, S., Goldberger, B. A., Ghani, M. A., Martin, D. M., Hu, H., & Gold, M. S. (2014). Prevalence of drug and alcohol use in urban Afghanistan: epidemiological data from the Afghanistan National Urban Drug Use Study (ANUDUS). The Lancet Global Health, 2(10), e592-e600.
De Matos, M. B., de Mola, C. L., Trettim, J. P., Jansen, K., da Silva, R. A., Souza, L. D., … & Quevedo, L. D. A. (2018). Psychoactive substance use s and dependence and its association with anxiety disorders: a population-based study of young adults in Brazil. Brazilian Journal of Psychiatry, 40(4), 349–353.
Daley, D. C., Smith, E., Balogh, D., & Toscaloni, J. (2018). Forgotten but not gone: The impact of the opioid epidemic and other substance use disorders on families and children. Commonwealth, 20(2–3). https://doi.org/10.15367/com.v20i2-3.189https://doi.org/10.15367/com.v20i2-3.189
Daley, D. C. (2013). Family and social aspects of substance use disorders and treatment. Journal of food and drug analysis, 21(4), S73-S76. https://doi.org/10.1016/j.jfda.2013.09.038.https://doi.org/10.1016/j.jfda.2013.09.038
Englander, H., Weimer, M., Solotaroff, R., Nicolaidis, C., Chan, B., Velez, C., … & Hartnett, T. (2017). Planning and designing the Improving Addiction Care Team (IMPACT) for hospitalized adults with substance use disorder. Journal of hospital medicine, 12(5), 339–342. https://doi.org/10.12788/jhm.2736.https://doi.org/10.12788/jhm.2736
Enkema, M. C., & Bowen, S. (2017). Mindfulness practice moderates the relationship between craving and substance use in a clinical sample. Drug and Alcohol Dependence, 179, 1–7. https://doi.org/10.1016/j.drugalcdep.2017.05.036https://doi.org/10.1016/j.drugalcdep.2017.05.036
Fielenbach, S., Donkers, F. C., Spreen, M., & Bogaerts, S. (2018). Effects of a theta/sensorimotor rhythm neurofeedback training protocol on measures of impulsivity, drug craving, and substance use in forensic psychiatric patients with substance use: Randomized controlled trial. JMIR mental health, 5(4), e10845. https://doi.org/10.2196/10845.https://doi.org/10.2196/10845
Fadardi, J. S., Ziaee, S.S.; & Barerfan, Z. (2008). The Persian Post-Detoxification Craving and Temptation Scale. Unpublished Manual, Ferdowsi university Mashhad.
Fadardi J. S., Ziaee S. (2009). Effect of attention control training program on the Iranian drug user. Unpublished manuscript, Mashhad, Ferdowsi.
Fadardi, J. S. (2003). Motivational and cognitive determinants of attentional bias for alcohol-related stimuli: implications for a new attentional-training intervention, Doctoral dissertation, University of Wales, Bangor.
Fadardi, J. S., Bar Arfan, Z., Amin Yazdi, A. (2010). The effect of Drugs-Attention Control Training Program on Drug-Related Attentional Bias and Improving other Indices of Recovery. Research in Clinical Psychology and Counseling, 11 (2): 29–56. Doi: 10.22067/IJAP.V11I2.807610.22067/IJAP.V11I2.8076
Griffin N, Khoshnood K (2010). Opium trade, insurgency, and HIV/AIDS in Afghanistan: relationships and regional consequences. Asia Pacific Journal of Public Health, 22(3 Suppl),159S–167S
Hazlett-Stevens, H., Zucker, BG, & Craske, MG (2002). The relationship of thought-action fusion to pathological worry and generalized anxiety disorder. Behavior Research and Therapy, 40 (10), 1199–1204. https://doi.org/10.1016/S0005-7967(01)00138-3https://doi.org/10.1016/S0005-7967(01)00138-3
Hagen, R., Hjemdal, O., Solem, S., Kennair, L. E. O., Nordahl, H. M., Fisher, P., & Wells, A. (2017). Metacognitive therapy for depression in adults: a waiting list randomized controlled trial with six months follow-up. Frontiers in Psychology, 8, 31. https://doi.org/10.3389/fpsyg.2017.00031https://doi.org/10.3389/fpsyg.2017.00031
Holman, R. C. (2004). Emotion and motive Effects on Drug-Related cognition. In Handbook of addictive disorders a practical guide to diagnosis and treatment. Newjersey: John Wiley & sons.
Kaviani, H., Mousavi, A. S. (2008). Psychometric properties of the Persian version of Beck Anxiety Inventory (BAI). Tehran University Medical Journal, 66 (2),136–140.
Koç, V., & Kafa, G. (2019). Cross-Cultural Research on Psychotherapy: The Need for a Change. Journal of Cross-Cultural Psychology, 50(1), 100–115. https://doi.org/10.1177/0022022118806577https://doi.org/10.1177/0022022118806577
Lakshmi, J., Sudhir, P. M., Sharma, M. P., & Math, S. B. (2016). Effectiveness of metacognitive therapy in patients with social anxiety disorder: A pilot investigation. Indian journal of psychological medicine, 38(5), 466–471. https://doi.org/10.4103/0253-7176.191385https://doi.org/10.4103/0253-7176.191385
Langenbach, T., Spönlein, A., Overfeld, E., Wiltfang, G., Quecke, N., Scherbaum, N., … & Hebebrand, J. (2010). Axis I comorbidity in adolescent inpatients referred for treatment of substance use disorders. Child and adolescent psychiatry and mental health, 4(1), 1–9.
McHugh, R. K., Hearon, B. A., & Otto, M. W. (2010). Cognitive behavioral therapy for substance use disorders. Psychiatric Clinics, 33(3), 511–525.
Moreno-Rius, J., & Miquel, M. (2017). The cerebellum in drug craving. Drug and alcohol dependence, 173, 151–158. https://doi.org/10.1016/j.drugalcdep.2016.12.028https://doi.org/10.1016/j.drugalcdep.2016.12.028
Mozafarinia, R., Assarian, M., & Ziaaddini, A. (2017). Prevalence of substance use among students of Tehran University of Medical Sciences, Iran. Addiction & Health, 9(2), 103.
Mokhtari, M., Hassanzadeh, R., & Mirzaeeyan, B. (2019). The Effectiveness of Meta-cognitive Skills Training on the Motivational Structure and Academic Performance of Drop-out Students. International Clinical Neuroscience Journal, 7(1), 46–51.
Normann, N., & Morina, N. (2018). The efficacy of metacognitive therapy: a systematic review and meta-analysis. Frontiers in Psychology, 9, 2211. https://doi.org/10.3389/fpsyg.2018.02211https://doi.org/10.3389/fpsyg.2018.02211
Normann, N., Van Emmerik, A. A., & Morina, N. (2014). The efficacy of metacognitive therapy for anxiety and depression: A meta‐analytic review. Depression and anxiety, 31(5), 402–411.
Ottonello, M., Fiabane, E., Pistarini, C., Spigno, P., & Torselli, E. (2019). Difficulties in emotion regulation during rehabilitation for alcohol addiction: correlations with metacognitive beliefs about alcohol use and relapse risk. Neuropsychiatric disease and treatment, 15, 2917.
Öst, L. G. (2008). Efficacy of the third wave of behavioral therapies: A systematic review and meta-analysis. Behavior research and therapy, 46(3), 296–321.
Papageorgiou, C., & Wells, A. (2001). Metacognitive beliefs about rumination in recurrent major depression. Cognitive and Behavioral Practice, 8 (2), 160–164. https://doi.org/10.1016/S1077-7229(01)80021-3https://doi.org/10.1016/S1077-7229(01)80021-3
Papageorgiou, C., & Wells, A. (2003). An empirical test of a clinical metacognitive model of rumination and depression. Cognitive therapy and research, 27(3), 261–273.
Saulsman, L., Anderson, R., Campbell, B., Swan, A., & Sng, A. (2017). Working with Worry and Rumination: A Metacognitive Group Treatment Programme for Repetitive Negative Thinking. Perth: Centre for Clinical Interventions
Spada, M. M., Mohiyeddini, C. & Wells, A. (2008). Measuring metacognitions associated with emotional distress: Factor structure and predictive validity of the Metacognitions Questionnaire 30. Personality and Individual Differences, 45, 238–242. DOI: 10.1016/j.paid.2008.04.00510.1016/j.paid.2008.04.005
Spada, M. M., & Wells, A. (2009). A metacognitive model of problem drinking. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 16(5), 383–393.
Shirinzadeh Dastgiri, S., Ali Goodarzi, M., Rahimi, CH., & Naziri, GH. (2009). Study of factor structure validity and reliability of Metacognitive Questionnaire-30. Journal of Psychology, 12(4),445–461.
Skinner, M. D., & Aubin, H. J. (2010). Craving’s place in addiction theory: contributions of the major models. Neuroscience & Biobehavioral Reviews, 34(4), 606–623. https://doi.org/10.1016/j.neubiorev.2009.11.024https://doi.org/10.1016/j.neubiorev.2009.11.024
Spada, M. M., Caselli, G., & Wells, A. (2013). The metacognitive therapy approach to problem drinking. New York: Harbringer.
Spada, M.M., & Wells, A. (2008). Metacognitive beliefs about alcohol use: Development and validation of two self-report scales. Addictive Behaviors, 33, 515–527.
Stefan-Dabson, K., Mohammadkhani, P., Massah-Choulabi, O. (2007). Psychometrics Characteristic of Beck Depression Inventory-II in Patients with Major Depressive Disorder. Rehabilitation, 8: 80–86.
Toneatto, T. (1999). Metacognition and substance use. Addictive behaviors, 24(2), 167–174.
Todd, C. S., Macdonald, D., Khoshnood, K., Mansoor, G. F., Eggerman, M., & Panter-Brick, C. (2012). Opiate use, treatment, and harm reduction in Afghanistan: recent changes and future directions. International Journal of Drug Policy, 23(5), 341–345.
UNODC. (2010b). Drug Use in Afghanistan: 2009 Survey Executive Summary. UNODC, Kabul, Afghanistan
Ward, ch., & Byrd, W. (2004). Word Bank Report: Afghanistan’s’ Opium Drug Economy. World Bank, Washington D.C: South Asia Poverty Reduction and Economic Management.
Wells, A., Fisher, P., Myers, S., Wheatley, J., Patel, T., & Brewin, C. R. (2012). Metacognitive therapy in treatment-resistant depression: A platform trial. Behavior research and therapy, 50(6), 367–373. https://doi.org/10.1016/j.brat.2012.02.004https://doi.org/10.1016/j.brat.2012.02.004
Wells, A. (2006). The metacognitive model of worry and generalized anxiety disorder. Worry and its psychological disorders: Theory, assessment, and treatment, 179–199.
Wells, A. (2011). Metacognitive therapy for anxiety and depression: The Guilford Press
Wells, A., & Sembi, S. (2004). Metacognitive therapy for PTSD: A preliminary investigation of a new brief treatment. Journal of behavior therapy and experimental psychiatry, 35(4), 307–318. https://doi.org/10.1016/j.jbtep.2004.07.001https://doi.org/10.1016/j.jbtep.2004.07.001
Wolitzky-Taylor, K., Krull, J., Rawson, R., Roy-Byrne, P., Ries, R., & Craske, M. G. (2018). A randomized clinical trial evaluating the preliminary effectiveness of an integrated anxiety disorder treatment in substance use disorder specialty clinics. Journal of consulting and clinical psychology, 86(1), 81–88. https://doi.org/10.1037/ccp0000276https://doi.org/10.1037/ccp0000276
Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy, 42, 385–396. DOI: 10.1016/S0005–7967(03)00147–510.1016/S0005–7967(03)00147–5
Wang, Y. P., & Gorenstein, C. (2013). Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Brazilian Journal of Psychiatry, 35, 416–431.
Yaghobi AsgharAbad, E., Bassak Nejad, S., Mehrabi Zade Honarmand, M., Zamiri Nejad,S. (2013). Effectiveness of metacognitive therapy (MCT) on depressed addicts under methadone maintenance treatment (MMT) in the city of Mashhad of Iran. Journal of North Khorasan University of medical science, 5 (1),167–174.