Introduction
Globally, alcohol is the leading risk factor for burden of disease in people aged 15–49 years (GBD 2016 Risk Factors Collaborators, 2017). Muslim-majority countries (MMCs) have the lowest prevalence of alcohol consumption globally because of the Islamic prohibition of alcohol (Alcohol Public Policy Group, 2010). Despite this, the consumption pattern among drinkers in some Eastern Mediterranean MMCs is the second-highest in risk globally (in terms of hazard per liter of alcohol consumed) (WHO, 2006a). Studies from the region suggest that youth in MMCs are exposed to alcohol despite their cultures’ discouragement of it. For example, there was a marked increase in student drinking in post-civil war Lebanon from 1991 to 1999, particularly among females (40.7% to 67.7%) (E. G. Karam, Maalouf, & Ghandour, 2004). There is also evidence of youth exposure to alcohol in Iran (Ṣirāmī, Qurbānī, & Mīnūnī, 2013) and among Palestinians in Israel, where even abstinent older people disclosed that they used to drink in their younger years (Baron-Epel et al., 2015; Yazbek et al., 2014). Furthermore, college students worldwide, including in MMCs, are a high-risk group for heavy drinking and alcohol-related problems (Hamdieh, Motalebi, Asheri, & Boroujerdi, 2008; E. Karam, Kypri, & Salamoun, 2007).
Iraq is an upper-middle-income country with an estimated population of over 38 million, of which the majority (60%) are younger than 24 years (UNDESA, 2017). Current alcohol policy in Iraq is inconsistent. The latest complete alcohol law passed in 2001. This policy provides clear regulations on the consumption and sale of alcoholic beverages (Al Ansari, Dawson, & Conigrave, 2019). Several provinces have also initiated their own policies since the invasion of Iraq beginning in 2003, when Western coalition forces toppled the decades-old rule of the Baathist Party and Saddam Hussein. These policies are still in practice despite an apparent alcohol ban in 2016. Alcohol remains available in Iraq and no clear alcohol policies or regulations are implemented (Al-Ansari, Thow, Day, & Conigrave, 2016).
Internationally, alcohol and drug use data for Iraq are based on expert estimates rather than surveys (WHO, 2010) and the majority of alcohol use in Iraq is believed to be unrecorded (WHO, 2014). Previous studies in Iraq have indicated differing figures regarding the prevalence of alcohol use. For example, in an unpublished study from 2014, the lifetime prevalence of alcohol use in Baghdad was reported to be 17.8% and increasing (N. J. Al-Hemiary, Al-Diwan, Hasson, & Rawson, 2014). In the same year, the Survey of Substance Abuse in Iraq (SSAI) suggests that half that number (8.6%; 16.7% male) were lifetime consumers (US Department of State, Bureau of International Narcotics and Law Enforcement Affairs, Iraqi Society of Addiction Medicine, University of California LA, & Center for Human Services, 2015). Even this is a marked increase on an earlier national household study, the 2006 Iraqi Mental Health Survey (IMHS), which found only 3.7% (6.8% of males) consumed alcohol in their lifetime. However, both national household studies report negligible alcohol use prevalence among females (0.6% in both studies) (US Department of State et al., 2015; WHO, 2009).
Despite the relatively low prevalence of alcohol use in the general population, risky drinking patterns are common among drinkers (Al Ansari, Dawson, & Conigrave, 2022). For example, the SSAI indicates that, on average, current drinkers consume more than six drinks per day on 10.5 days a month. Two thirds (70%) of current drinkers in the general population scored within the dependence range on the Severity of Substance Dependence Scale (SDS) (US Department of State et al., 2015). Interestingly, the national Iraqi Mental Health Survey (IMHS) from just ten years prior reported a very low prevalence of alcohol abuse in the general population (0.1%; using the Composite International Diagnostic Interview 3rd edition CIDI-3) (WHO, 2009). In contrast, a specialized sample from youth centers in Baghdad found that 17% of more than 2000 attendees met criteria for alcohol abuse (using CIDI-2) with an average onset age of 21.7 years (Al-Diwan, Al-Hemiary, & Hashim, 2015; N. Al-Hemiary, Hashim, Al-Diwan, & Abdul Razzaq, 2015).
Alcohol Consumption Among University Students in Iraq
Worldwide, university student drinking is a major health concern, including in some MMCs such as Lebanon and Egypt (E. Karam et al., 2007; E. G. Karam et al., 2004). However, a systematic review of alcohol literature in the Arab world identified a scarcity of literature about youth and student drinking in Iraq (Ghandour et al., 2016).
The 2014 Iraqi household study (SSAI) included 230 students (not specified if they were university students) and reported that fewer than one in 30 students had ever consumed alcohol (3.0%) and fewer than one in 50 were current drinkers (1.7%) (US Department of State et al., 2015). An earlier 2010 study in Karbala indicated a similarly low prevalence of current drinking among 5446 students (2.2%; male 4.1%; female 0.4%) (Al Mousawi, 2015).
By contrast, in the large metropolis of Baghdad, results differ across studies. The lifetime consumption of alcohol was over four times higher among three Baghdadi universities than national or Karbala prevalence (9.7%; 19.7% male; 0.8% female) (Al-Ameri, Al-Badri, & Lafta, 2016). However, data collected at around the same time from medical students at Baghdad University indicated a far lower prevalence at 0.4% (the authors did not specify if this is lifetime or current drinking) (Al-Imam, Al-Mukhtar, Shafiq, & Irfan, 2017).
In an earlier (2007) survey in Erbil, a city in Iraqi Kurdistan, the prevalence of drinking (in the past six months) was even higher: Double the prevalence reported at the three Baghdadi universities (23.7% among 342 students; 34.7% male; 4.1% female) (S. Ali & Sabir, 2009). The tool used to collect the consumption data is not described. In keeping with this prevalence, a study about student risky behavior seven years later at the same university indicated that over a tenth (10.9%) of a sample of 211 students reported having driven a vehicle under the influence of alcohol (Shabila, Ismail, Saleh, & Al-Hadithi, 2015).
It is not clear why the prevalence of consumption has varied so greatly in previous studies among student populations in Iraq. Potential reasons for variability include the method of survey administration and degree of privacy. Surveys often use interviews or paper surveys in a controlled setting (e.g., classroom or in-home), where it can be challenging to guarantee confidentiality. Only one study (about novel psychoactive substances, but including self-report alcohol questions) used an online questionnaire (Al-Imam et al., 2017). The fact that samples are derived from single universities or single cities also makes it hard to generalize findings.
Identifying alcohol use, attitudes, and perceived motives for drinking among students allows for an assessment of their vulnerability. We were only able to identify two studies in local journals that assessed attitudes toward ‘addiction’ in general and medical samples (Al-Hasnawi, 2006; Al-Hasnawi, Al-Hemiary, & Lafta, 2007; Al Ansari et al., 2022). To our knowledge, there is currently no literature about attitudes to alcohol consumption and alcohol policy in Iraq among Iraqi university students.
To address the challenges of social desirability bias, and collect data on alcohol more sensitively and accurately, we used online data collection, designed to maximize anonymity and confidentiality. We recruited students from multiple universities around Iraq to increase generalizability. We also collected data on perceived motives for drinking, attitudes on drinking and drinkers, attitudes on various alcohol policies, and a possible connection between war or media exposure and alcohol use. Assessing these attitudes are important in understanding current behavior and potential coming trends. It is hoped that this study will help inform policy and preventative measures in Iraq and other MMCs.
Methods
An online cross-sectional survey of Iraqi university students was conducted as the quantitative component of a larger mixed-method study on attitudes of university students in Iraq toward alcohol.
Ethics Approval
Ethics approval was granted by the Medical Ethics Committee at the College of Medicine in the University of Kufa, Iraq (MECCM-0028).
Quantitative Survey
The survey included 42 questions that were derived from household and college surveys from other countries, mainly Australia and Sweden (Australian Institute of Health and Welfare, 2013; Bullock, 2004). These were edited to suit the local context in consultation with local collaborators and international experts. A draft Arabic translation of the survey was produced and then finalized in consultation with local recently graduated medical doctors in a focus group. The survey was piloted in English and Arabic by members of this focus group and took 15–20 minutes to complete. The Arabic survey was also shared with religious and cultural elders for comment. Based on these comments, some minor changes to the Arabic translation of the survey were made.
Following a consent question, demographic items enquired into the student’s family and university background, including internal displacement status and living situation. The participants were also asked “what is your religious affiliation?” [Arabic: mā hīya dīyānatuk?] and “what ethnicity do you identify as?” [Arabic: mā huwa āṣluk al-ʿirqī?]. Both questions allowed the participant to choose how they identify from a list of the most common religious and ethnic groups in Iraq, including an “other” free-text option.
Participants were then asked if they had ever consumed alcohol and were screened using the AUDIT-C tool (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998). This three-item tool, comprised of the first three items of the AUDIT questionnaire (T. F. Babor, Higgins-Biddle, Saunders, & Monteiro, 2001), asks about frequency, amount of usual drinking, and frequency of drinking six or more drinks (Bradley et al., 1998; Kelly, Donovan, Chung, Bukstein, & Cornelius, 2009). Past or current drinkers were then asked about their drinking location, source of alcohol, and who they consumed it with. Non-drinkers were asked about any desire to consume alcohol in the future. These alcohol questions were followed by questions regarding use of other substances. Common substances used in Iraq were identified using literature and in consultation with local collaborators.
Additional items in the survey inquired into attitudes toward alcohol and other drug consumption and policies. Participants were then asked about exposure to alcohol in the media, and about exposure to war and violent conflict, before being screened for post-traumatic stress disorder (PTSD) using the four-item primary care PTSD (PC-PTSD) screening tool. This tool was chosen due to its brevity (Prins et al., 2003) and suitability for a general population.
To maximize anonymity and confidentiality, and to minimize social desirability bias, the questionnaire was delivered as an anonymous online survey using the SurveyGizmo platform. No identifying information or trackable IP addresses were collected.
Sampling and Recruitment
A mixture of convenience and snowball sampling was used to recruit participants. These were chosen as viable approaches to online recruitment for such a sensitive topic. Furthermore, there were limited central databases of student emails within universities in Iraq and therefore random online sampling would have been difficult. The survey was open for online participation from 5th of March to 5th of May 2017, although active recruitment only took place from the 8th to the 31st of March 2017. Senior academic representatives of three Iraqi universities gave permission for their students to be recruited. Initial recruitment took place online via the e-learning platform of one of the universities, with lecturers encouraging their students to take part in the survey. However, it was mentioned by students and staff that other faculties and universities often did not actively use their e-learning platforms and that student communication online occurred via student-only social-media groups. Accordingly, further recruitment was carried out via these social media groups. As this study was conducted concurrently with the qualitative component of the larger mixed-method project, interview participants were also asked to distribute the survey link to their student networks. Initial recruitment was commenced within the medical academic departments at each university (via academics, students, and other consultants), and then expanded to other faculties via students and staff contacts. Names of the universities will not be reported because of the sensitivity of alcohol in an MMC setting.
The only inclusion criteria for the survey were to be a consenting current student at an Iraqi university and aged under 24 years. Students could choose to complete the survey in Arabic or English.
Data Analysis
Data were downloaded from SurveyGizmo, then analyzed using SPSS Statistics 25. The data was cleaned and participants who either reported themselves to be not current students at an Iraqi university, to be above the age of 24, or who had not provided any information regarding their alcohol consumption were excluded. Drinkers were classified as at risk if the sum of the AUDIT-C items was three or more for females and four or more for males (Dawson et al. 2012). Those that answered yes to three or more questions on the PC-PTSD tool were scored positive for this screen (Prins et al., 2003).
Chi square tests were used to compare consumption patterns between different demographic groups (e.g., by age, gender, religion, and living location). Fisher’s exact test was used if expected cell values were less than four. Significance was tested based on p value of less than 0.05. Predictors that were significant in the bivariate analysis were considered for inclusion in a multivariate logistic regression analysis to determine their independent predictive effect. As a significant majority of our sample were Muslims, a further bivariate and multivariate analysis was conducted to determine demographic factors associated with drinking in this subgroup.
Results
Sample
A total of 652 people accessed the survey link. Of those, 525 were eligible (students between the ages of 17 and 24 years old), consented to the terms of the study, and started the survey. Of that subgroup, 468 participants (89%) answered at least one consumption question and were included in further analysis. The alcohol and drug consumption, availability, and use section was completed in full by 448 participants. However, only 192 students (36.6% of eligible participants) completed the entire survey (Table 1). Each table and figure only include the individuals who answered that specific question or section. There was no association between ever drinking and failure to complete the full questionnaire.
Students responded in either Arabic (n = 388) or English (n = 80).
Number of participants completing the different survey sections
| Eligible | Provided any alcohol data | Completed alcohol/drug use section | Completed attitudes section | Completed war & media section | |
|---|---|---|---|---|---|
| Respondents (n) | 525 | 468 | 448 | 220 | 192 |
| Percent (%) | 100% | 89% | 85% | 42% | 37% |
Demographics
Students were aged between 17 and 24 (mean = 20.52 years, standard deviation [sd] = 1.43). Over half of the sample was female (n = 258; 55.1%). The participating students were from more than ten Iraqi universities, but most attended four large public universities in four different provinces in Iraq. Students were from a broad range of regions across Iraq. However, despite repeated attempts at recruitment, no university from the Kurdistan region participated. The majority (n = 368; 78.6%) of participants were students in faculties of medicine, followed by 9.6% (n = 45) from faculties of pharmacy. Of the 468 students who provided alcohol data, 450 (96.2%) were undergraduate students, eight were postgraduate, and ten did not specify.
Islam was the predominant religion (n = 448, 95.7%) reported. The majority (76.9%; n = 360) of respondents reported living with relatives, while 23.1% (n = 108) lived alone, in dormitories, or with friends. Most (78%; n = 355) students reported their socioeconomic level between steps 4 and 7 on a ten-step socioeconomic ladder. Internally displaced people accounted for 15.8% of the sample (n = 74).
Alcohol Consumption
Just over one in twenty (5.3%) students had ever consumed alcohol (n = 25); the majority of those were male (n = 21) and non-Muslim (n = 15). Consumption in the last 12 months was only slightly less common (4.5%; n = 21 of students). However, three of these 21 students with recent consumption later indicated that they “never” consumed alcohol when asked, “How often do you have a drink containing alcohol” on AUDIT-1. Of the non-drinkers, 88% (n = 373) reported not having any desire to try alcohol in the future.
Six of the 15 males who had consumed alcohol in the past year scored above four in the AUDIT-C (40%). None of the four women scored above three. On average, the onset of drinking was at the age of 17.83 (sd = 3.96). Males, older students (21–24 years), non-Muslims, non-Arab respondents, and those in a relationship outside of marriage or living away from parents were more likely to have consumed alcohol (lifetime and past-year; Table 2).
Prevalence of lifetime and past-year alcohol consumption by selected demographic data
| Lifetime abstinence | Lifetime use | Past-year use | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | p-value | n | % | p-value^ | Total n | % | |
| Age | ||||||||||
| 17–20 | 233 | 97.5 | 6 | 2.5 | 0.005* | 4 | 1.7 | 0.003* | 239 | 51.1 |
| 21–24 | 210 | 91.7 | 19 | 8.3 | 17 | 7.4 | 229 | 48.9 | ||
| 468 | 100 | |||||||||
| Gender | ||||||||||
| Male | 189 | 90.0 | 21 | 10 | <0.001* | 17 | 8.1 | 0.001* | 210 | 44.9 |
| Female | 254 | 98.4 | 4 | 1.6 | 4 | 1.6 | 258 | 55.1 | ||
| 468 | 100 | |||||||||
| University | ||||||||||
| University A | 211 | 96.8 | 7 | 3.2 | 0.028* | 4 | 1.8 | 0.011* | 218 | 46.6 |
| University B | 42 | 100 | 0 | 0 | 0 | 0 | 42 | 9 | ||
| University C | 50 | 87.7 | 7 | 12.3 | 6 | 10.5 | 57 | 12.2 | ||
| University D | 90 | 92.8 | 7 | 7.2 | 7 | 7.2 | 97 | 20.7 | ||
| Other | 50 | 92.6 | 4 | 7.4 | 4 | 7.4 | 54 | 11.5 | ||
| 468 | 100 | |||||||||
| Faculty | ||||||||||
| Medicine | 346 | 94.0 | 22 | 6.0 | 0.361 | 18 | 4.9 | 0.422 | 368 | 78.6 |
| Pharmacy | 44 | 97.8 | 1 | 2.2 | 1 | 2.2 | 45 | 9.6 | ||
| Engineering | 23 | 92.0 | 2 | 8.0 | 2 | 8.0 | 25 | 5.3 | ||
| Other | 30 | 100 | 0 | 0 | 0 | 0 | 30 | 6.4 | ||
| 468 | 100 | |||||||||
| Step on socioeconomic ladder# | ||||||||||
| 1–3 | 32 | 97.0 | 1 | 3.0 | 0.638 | 0 | 0 | 0.242 | 33 | 7.3 |
| 4–7 | 336 | 94.6 | 19 | 5.4 | 16 | 4.5 | 355 | 78.0 | ||
| 8–10 | 62 | 92.5 | 5 | 7.5 | 5 | 7.5 | 67 | 14.7 | ||
| Missing | 13 | 2.8 | ||||||||
| 468 | 100 | |||||||||
| Religion | ||||||||||
| Muslim | 438 | 97.8 | 10 | 2.2 | <0.001* | 8 | 1.8 | <0.001* | 448 | 95.7 |
| Non-Muslim | 5 | 25 | 15 | 75 | 13 | 65 | 20 | 4.3 | ||
| 468 | 100 | |||||||||
| Ethnicity | ||||||||||
| Arab | 415 | 95.6 | 19 | 4.4 | 0.001* | 15 | 3.5 | <0.001* | 434 | 92.7 |
| Non-Arab | 28 | 82.4 | 6 | 17.6 | 6 | 17.6 | 34 | 7.3 | ||
| 468 | 100 | |||||||||
| Relationship status | ||||||||||
| Single | 393 | 95.2 | 20 | 4.8 | 0.002* | 16 | 3.9 | <0.001* | 413 | 89.6 |
| Unmarried couple | 19 | 79.2 | 5 | 20.8 | 5 | 20.8 | 24 | 5.2 | ||
| Married or engaged | 24 | 100 | 0 | 0 | 0 | 0 | 24 | 5.2 | ||
| Missing | 7 | 1.5 | ||||||||
| 468 | 100 | |||||||||
| Internally displaced? | ||||||||||
| Yes | 68 | 91.9 | 6 | 8.1 | 0.249 | 6 | 8.1 | 0.101 | 74 | 15.8 |
| No | 375 | 95.2 | 19 | 4.8 | 15 | 3.8 | 394 | 84.2 | ||
| 468 | 100 | |||||||||
| Living location | ||||||||||
| With parent, partner, or relative | 347 | 96.4 | 13 | 3.6 | 0.002* | 10 | 2.8 | 0.001* | 360 | 76.9 |
| Alone, dorms, or with friends | 96 | 88.9 | 12 | 11.1 | 11 | 10.2 | 108 | 23.1 | ||
| 468 | 100 | |||||||||
* p-value less than 0.05
-
^ the p-statistics for past-year use are in comparison to past-year abstinence (not shown)
-
# the SES ladder allowed students to position themselves in Iraqi society on a ten-step socioeconomic ladder.
Four of the five dichotomous variables that were significant in the bi-variate analysis were included in the multivariate analysis (except non-Arab as closely correlated to non-Muslim). The multivariate logistic regression model confirmed that being a non-Muslim was the most significant independent predictor (p < 0.001) for lifetime and past-year drinking. Living away from relatives was also an independent predictor for lifetime and past-year consumption (Table 3). However, being older was only a significant independent significant predictor for past-year consumption while being male was only significant for lifetime consumption.
Independent predictors of consumption (using logistic regression)
3a. Independent predictors of lifetime consumption (n = 468)
| Wald | Df | Sig. | Odds ratio (95% CI) | |
|---|---|---|---|---|
| Older (21–24 years) (vs. 17–20 years) | 3.214 | 1 | 0.073 | 3.34 (0.89–12.49) |
| Male (vs. female) | 6.586 | 1 | 0.010 | 7.29 (1.60–33.21) |
| Live alone, with friends, or university dorm (vs. live with parents, partner, or relatives) | 5.504 | 1 | 0.019 | 4.12 (1.26–13.42) |
| Non-Muslim (vs. Muslim) | 45.838 | 1 | < 0.001 | 202.43 (43.51–941.69) |
| Constant | 45.271 | 1 | < 0.001 | 0.002 |
3b. Independent predictors of past-year consumption (n = 468)
| Wald | Df | Sig. | Odds ratio (95% CI) | |
|---|---|---|---|---|
| Older (21–24 years) (vs. 17–20 years) | 4.613 | 1 | 0.032 | 4.99 (1.15–21.60) |
| Male (vs. female) | 3.431 | 1 | 0.064 | 3.85 (0.93–16.05) |
| Live alone, with friends, or university dorm (vs. live with parents, partner, or relatives) | 6.565 | 1 | 0.010 | 5.34 (1.48–19.23) |
| Non-Muslim (vs. Muslim) | 43.929 | 1 | < 0.001 | 140.51 (32.55–606.49) |
| Constant | 44.282 | 1 | < 0.001 | 0.001 |
Alcohol Consumption Among Muslim Students
A total of ten lifetime drinkers and eight current drinkers identified as Muslim (2.2% and 1.8% of Muslim students, respectively). Among the subset of students who were Muslim (n = 448), on bivariate analysis, lifetime consumption was significantly associated with older age (p = 0.042), living away from relatives (p = 0.011), and being male (p = 0.003). Past-year consumption was associated only with living away from relatives (p = 0.017) and being male (p = 0.024). When significant variables from bivariate analysis were controlled for in multivariate logistic regression, being a male (AOR = 8.48 [95%CI = 1.04–69.11]) and living away from relatives (AOR = 4.35 [95%CI = 1.17–16.14]) stayed significant for lifetime consumption of alcohol by Muslim students. However, only living away from relatives (AOR = 4.84 [95%CI = 1.11–21.02]) remained significant for past-year consumption.
Alcohol Availability and Student Perception of Alcohol use
A majority of students (54.9%) thought that it was easy or very easy for students to get alcohol if they wanted it, while only 15.3% reported it being very difficult or impossible; this perception was not significantly associated with lifetime or past-year consumption. Over half of the 20 respondents to the source of alcohol question (n = 13; 65%) reported that they get their alcohol from bottle shops. Over half (n = 11) of the 21 past-year alcohol consumers reported that they drink with their university colleagues. A quarter of all participants (n = 106/450) reported that they know of friends and/or family who use alcohol. However, of those, only 28 (6.2% of 450) reported that they know a university friend who consumes alcohol. Despite this, participants (n = 459) on average estimated that over a fifth (mean = 21.1%; SD 17.3) of university students in Iraq drink alcohol. Lifetime and past-year drinkers estimated a higher prevalence of student drinking than did non-drinkers (p < 0.001).
Consumption of other Substances
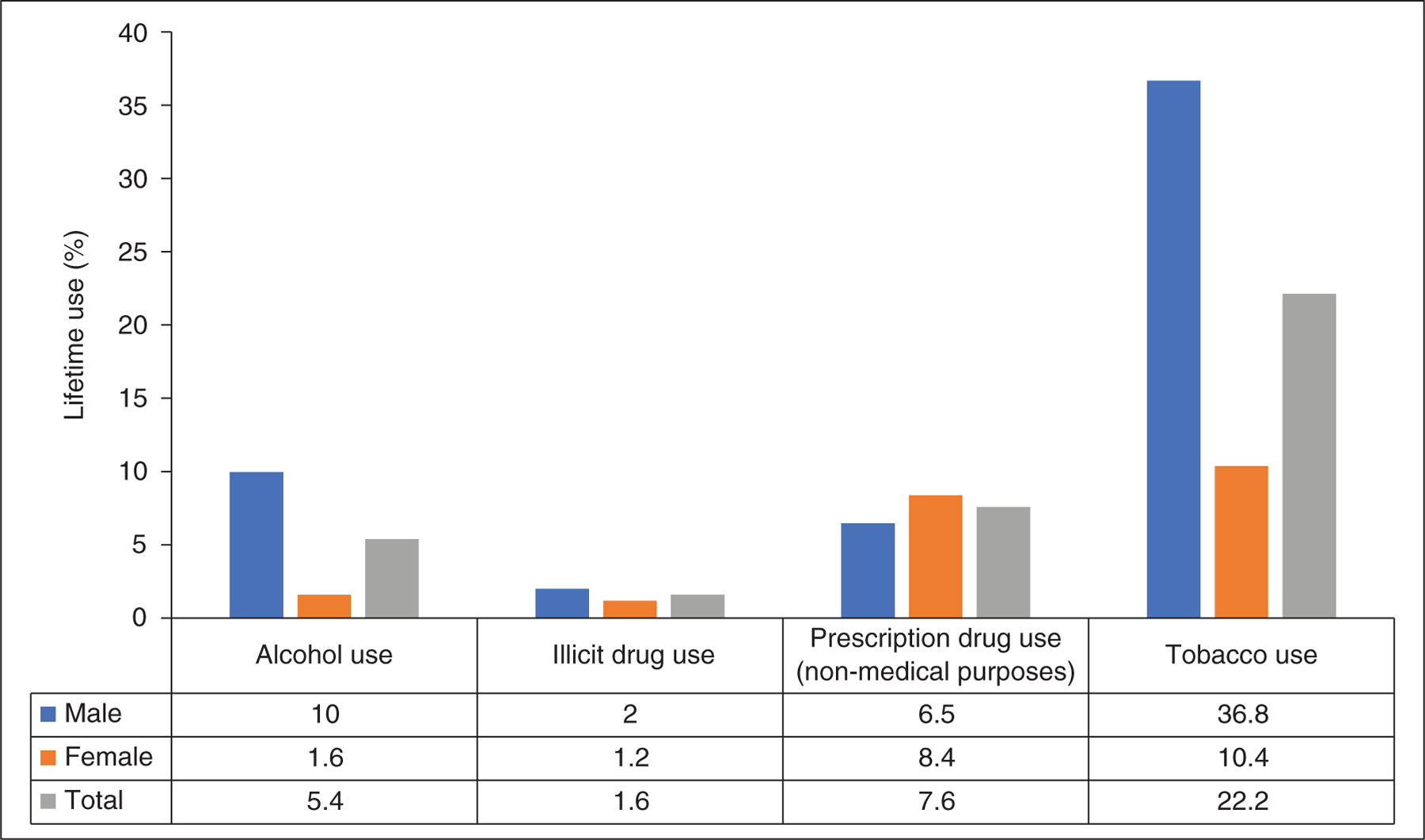
A total of 34 out of 450 respondents (7.3%: 6.5% male, 8.4% female) reported taking one or more prescription drugs (benzodiazepines, benzhexol, anti-depressants, anti-psychotics, painkillers, analgesics, or opioids) for non-medical/non-therapeutic reasons. Only seven (1.6%) reported lifetime illicit drug use. One in five participants (n = 100; 22.2%) reported tobacco use, with males representing three times as many users as female participants (36.8% and 10.4% respectively; figure 1).
Attitudes toward Alcohol, Alcohol Policy, and Alcohol/Drug users
When asked about motives for drinking or abstinence on a four-point Likert scale (never, rare, sometimes, and often), all students agreed that motives for drinking were sometimes/often perceived to be either a desire to try forbidden things (87.5%), experiences of trauma (85.7%), fun (82.7%), or peer pressure (81.2%). On the other hand, lack of religiosity was perceived as a motivating factor by 92.2% of non-drinkers compared to only two-thirds (66.7%) of lifetime drinkers (p = 0.006). Participants also perceived that sometimes/often students abstained for religious (93.7%), family (90.2%), and socio-cultural (89.7%) reasons. In comparison, fewer than half (44.4%) of lifetime drinkers and two thirds (69.2%) of non-drinkers perceived that abstinence was sometimes or often for health reasons (p = 0.029). When students (n = 257) were asked if alcohol is a moral issue, 67.7% agreed while only 43% agreed that it is a medical issue.
Of the participants (n = 256) who responded to the question asking whether they agree with certain alcohol policy options, nearly two thirds (n = 166; 65.1%) thought that alcohol should be prohibited entirely. However, 104 (40.8%) agreed with a policy that would allow alcohol production, trade, and consumption for non-Muslims in Iraq. A sixth of students (n = 42; 16.5%) agreed with a policy that alcohol production, sale, and consumption should be permitted for everyone.
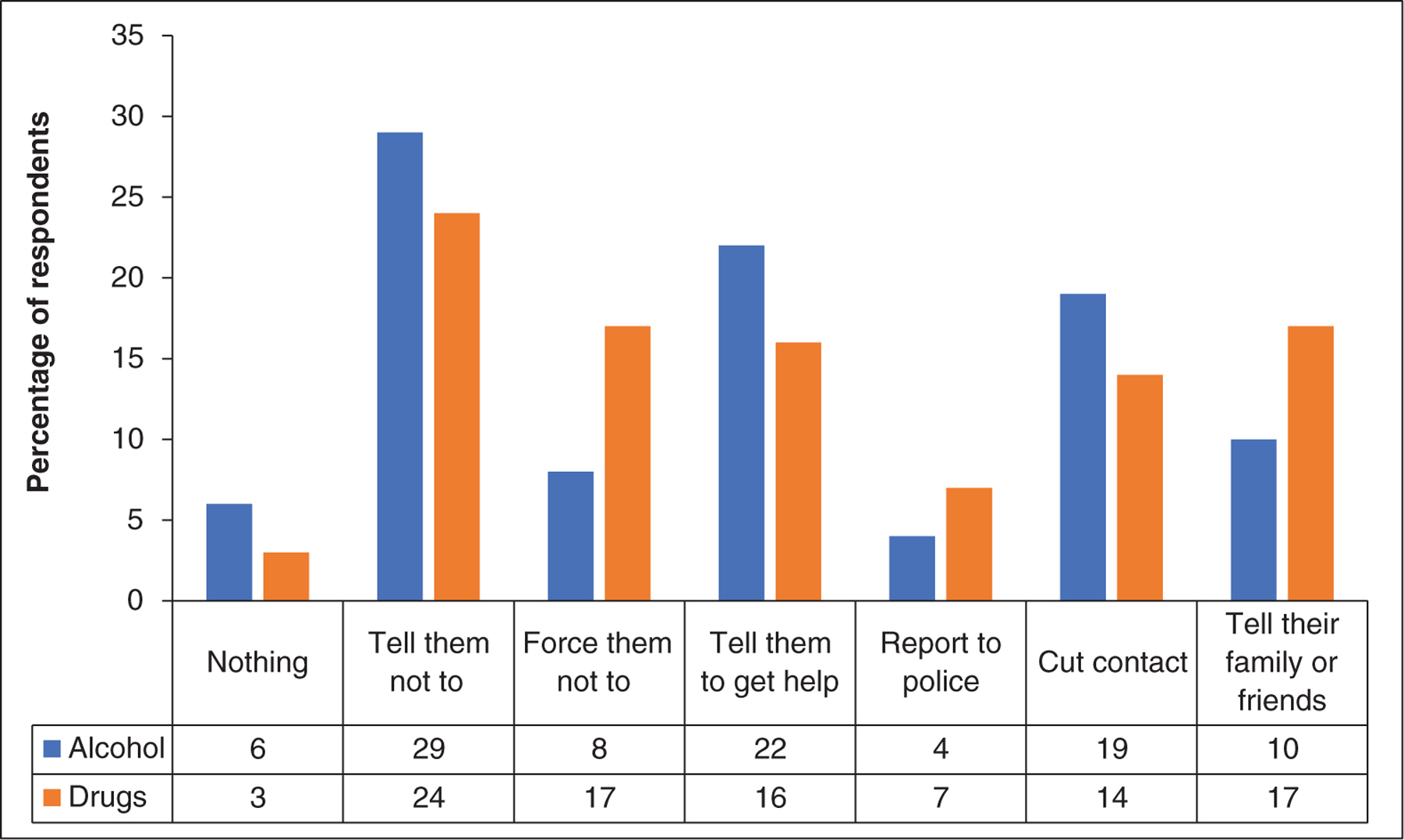
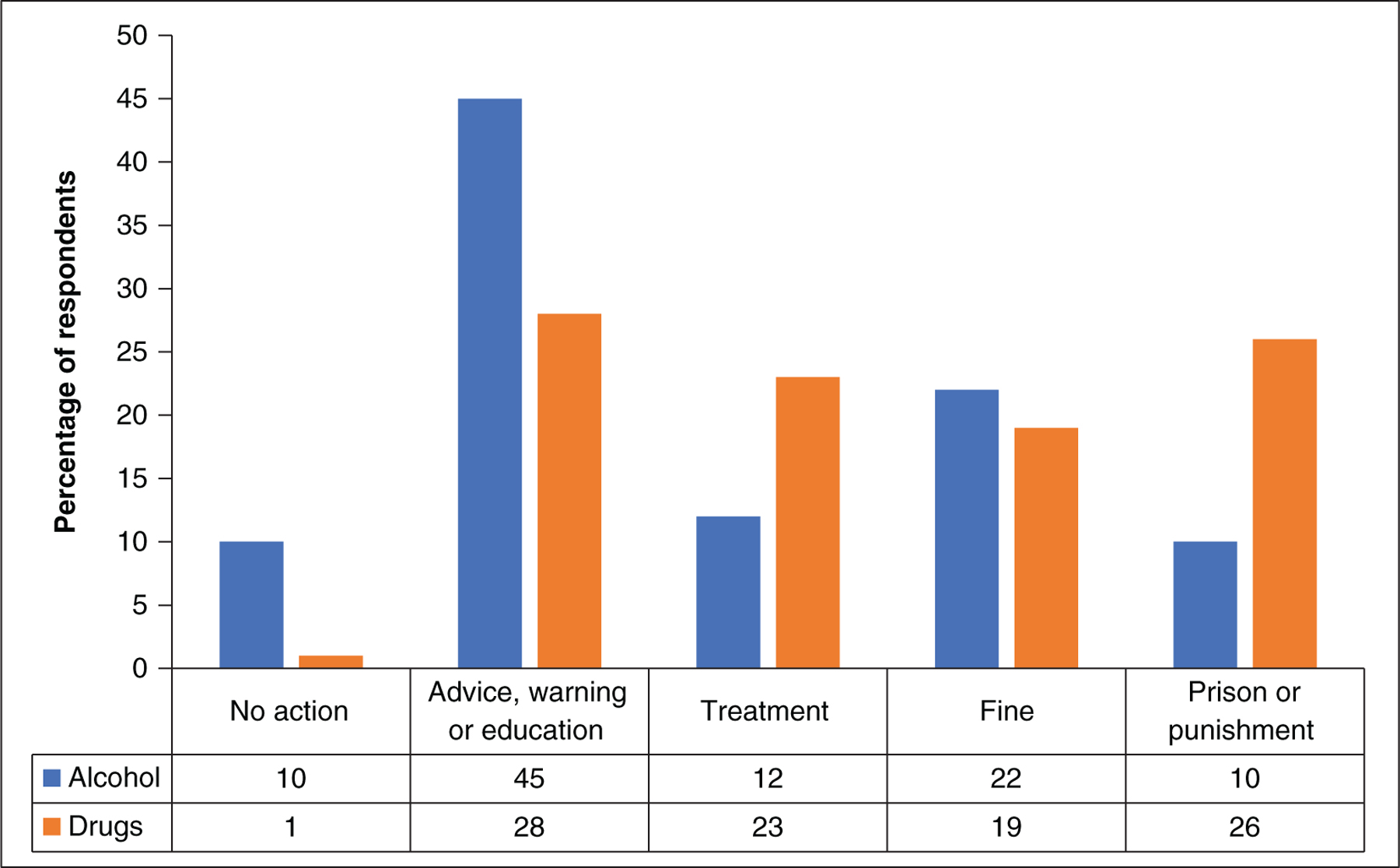
Students reported that their most likely action if they encountered a friend using either alcohol or drugs daily would be to advise them to stop (29.1% and 24.1%, respectively). More severe responses (force them not to; tell police, family, or friends) were more likely to be endorsed for drug use than for alcohol. A similar trend was observed when participants were asked what should happen if someone was caught with small amounts of alcohol or drugs (Figure 2).
Media and War Exposure, and Post-Traumatic Stress Disorder
Of the 202 students that were asked if they had been exposed to direct alcohol marketing, more than half had been exposed on the internet (n = 112; 55.4%), two fifths on social media (n = 84; 41.6%), and satellite TV (n = 72; 35.6%). A third of the sample indicated they have never had any exposure to alcohol advertisements (n = 74; 36.6%). There was a significant association between drinking status and perception of mass media (p = 0.035) and social media (p = 0.009) as factors contributing to drinking. Two thirds of non-drinkers perceived that mass media or social media influences drinking (n = 214, 66.7% and n = 212, 67.3%, respectively), only two-fifth (n = 6, 40%) and one-third (n = 5, 33.3%) of lifetime drinkers respectively agreed.
Of the 220 individuals who answered the questions on exposure to violent conflict and on PTSD symptoms, two in five (n = 90; 41.7%) reported direct experience of war or violent military conflict. Almost a third (n = 63;29.2%) of the respondents were positive on the PC-PTSD screening test. No significant association was found between PC-PTSD results and lifetime consumption. No past-year drinker (n = 9) scored positive on the PC-PTSD test.
Discussion
To our knowledge, this is the first comprehensive study to examine the behaviors and attitudes of young Iraqi university students toward alcohol and alcohol policy. This is also the most current data from university students across several regions in Iraq that provides insight into student exposure to alcohol, consumption patterns, and perceived availability. Our findings provide important insights for interventions to improve the collection of data about alcohol use and socio-cultural norms that can be used to reduce alcohol related risk factors.
Almost one in twenty students in our sample had consumed alcohol (lifetime: 5.4%; past-year: 4.6%). This is almost double the lifetime use reported by the 2014 national survey’s (SSAI) adult student sub-sample (3%) and thirteen times the prevalence (0.4%) among medical students surveyed at Baghdad University in 2016 (Al-Imam et al., 2017). In contrast, students in our sample were only half as likely to report lifetime consumption of alcohol as respondents in a three-university study in Baghdad (Al-Ameri et al., 2016). However, in this same study, a similar prevalence of drinking to our study was reported by medical students (6.0% vs. 5.3%) (Al-Ameri et al., 2016).
The different consumption rates identified in our research compared to those in other studies may be explained by contextual factors and the data collection methods. For example, Karbala is a conservative religious city while Erbil, the capital of Kurdistan, has a higher non-Muslim population and is more modernized than the Arab majority regions of Iraq. Correspondingly, Mousawi (2015) reported the prevalence of past-year drinking in Karbala to be 2.2%, which is half the rate of consumption identified in our study. In contrast, in Erbil, Ali and Sabir (2009) found that almost half (44%) of medical students living at colleges in Hawler Medical University had used alcohol in the past six months. This is four times the past-year consumption of medical students living away from family in our sample (10.4%) that did not include students from this location.
In contrast to our study that used an online questionnaire tool, nearly all previous studies collecting alcohol data in Iraq have used pen-and-paper or face-to-face data collection methods. These approaches have been found to affect the accuracy of self-reported drinking in non-MMCs cultures with sensitivities to alcohol (Islam et al., 2012). Pen-and-paper or face-to-face data collection methods have also been identified as limitations in the two Iraqi national household studies (US Department of State et al., 2015; WHO, 2009).
On average, students estimated the prevalence of drinking among their fellow students at four times the actual self-reported prevalence (21.1% vs. 5.4%). A quarter of participants reported knowing a friend or family member that drinks (23.6%). Similar high reports of knowing someone who drinks have been reported previously in Iraq (US Department of State et al., 2015). Lifetime and current drinkers estimated a higher prevalence of peer drinking than did non-drinkers. This may indicate that students under-reported their personal consumption. Alternatively, it may indicate an overestimation of student drinking norms by drinking participants. The overestimation of drinking norms has been shown to influence consumption in non-MMCs. Interventions to correct individual misconceptions of drinking prevalence have been shown to be effective in reducing problem drinking among students (Lewis & Neighbors, 2006; Ridout & Campbell, 2014). These interventions normally require identifying the at-risk drinkers in the first place – an unlikely possibility in Iraq where alcohol is a sensitive topic. In addition, due to the nature of the sensitivities, it is difficult to establish actual drinking norms. Students are also unlikely to trust figures presented because they may have themselves underreported their drinking or know someone who has.
Two fifths (20%) of male drinkers in our sample met the criteria for risky drinking (AUDIT-C score of 4+). In a 2010 study at Karbala University using the full 10-item AUDIT, more than half of drinking students (56%) reported consuming alcohol at risky levels (AUDIT score of 8+) (Al Mousawi, 2015). We purposely did not use the full AUDIT because the authors noted possible inflated scores resulting from items 7 and 10 of the AUDIT (guilt and others’ concern about drinking). This score inflation is consistent with the common anti-alcohol sentiment in MMCs. Further research is needed to identify culturally relevant ways to ask items relating to consequences of drinking – with consideration that guilt and social concern may be elevated in this setting.
The high prevalence of risky drinking patterns in Iraq is confirmed by two other studies: one in a national household study and the other in a specialized sample. Almost one in six males that attended youth centers in Baghdad met DSM-IV criteria for alcohol abuse using the Composite International Diagnostic Interview (CIDI-2) (N. Al-Hemiary et al., 2015). The SSAI reports that 71% of current drinkers met the criteria for dependence on the Severity of Substance Dependence Scale (SDS) (US Department of State et al., 2015). This may reflect the over-reporting of guilt/shame in item 3 of the SDS. WHO estimates show alcohol use patterns among drinkers in EMRO are second in risk to former soviet Eastern Europe (WHO, 2006b).
Our study is consistent with previous studies in reporting no risky drinking or alcohol misuse among females. Biological sex was associated with lifetime drinking but was no longer significant for past-year consumption in our multi-variate analysis. A strong association of alcohol use with males was identified in the national household survey (US Department of State et al., 2015) and other studies (Al-Ameri et al., 2016; Al Mousawi, 2015). However, female students in our study reported a higher consumption of alcohol (and other drugs). For example, compared to the SSAI, females in our sample provided higher reports of lifetime drinking (1.6% vs. 0.6%) and current alcohol use (1.6% vs. 0.11%). They also reported a higher prevalence of lifetime illicit drug use (1.2% vs. 0%) and licit drug misuse (8.4% vs. 0.7%) (US Department of State et al., 2015). This could be attributed to sampling differences or the greater anonymity of our data collection methods.
The gendered role that alcohol plays in Iraq and other MMCs may reflect socio-cultural norms. Haya’ (modesty or shyness) is a universal encouraged trait in Muslim societies particularly for females (M. Ali, 2014). Drinking is considered an immodest act in Islam and local cultures. Observing haya’ may also reduce risk factors associated with alcohol consumption. For example, Iraqi females seldom live or travel alone or with friends – most would stay with relatives even if they study away from home. Our data indicate that living alone, with friends or at university dormitory was significantly associated with being male (p = 0.01; data not shown) and in turn, significantly associated with drinking. Furthermore, when controlling for living away from relatives in the multivariate logistic regression, being a male was no longer an independent predictor of past year drinking, even among Muslim students. It is possible that being a male remained significant in lifetime consumption because the survey only asked about current living circumstances, and males are more likely to have lived or travelled away from home in the past. The association of drinking and living away from home was also observed in students in Baghdad (Al-Ameri et al., 2016) and in non-MMCs such as Sweden (Bullock, 2004). This indicates that there may be an opportunity to focus prevention efforts on students who live in dormitories or with friends.
Interactions between the sexes are also limited in Iraqi society, especially in conservative areas. In conservative settings, the university may be the only environment where females closely interact with their male peers. By observation, in some areas of Iraq, there can be a disparity between a student’s behavior at the university and their life in the family home. It is possible that these different lifestyles, the stress of studies, and the stigma around alcohol and illicit drug use may contribute to prescription drug use for non-medical reasons as observed in our female sample.
As indicated, two thirds (67.6%) of students agreed with the statement that alcohol is a moral issue (vs. 43% that agreed it was a medical issue). Similar observations have been made about attitudes toward “addiction” in Iraq (Al-Hasnawi, 2006; Al-Hasnawi et al., 2007). Students from our sample reported most abstain for religious, socio-cultural, and family purposes. They perceived that students in general mostly drink due to lack of religiosity, trauma, for fun, or because they find forbidden actions tempting. Student reactions to those who drink alcohol seem to also be driven by religious teachings or a sense of social and familial responsibility. For example, a fifth of the sample indicated they would cut off contact if a friend were using alcohol daily and more than half indicated they would either tell them to stop or to get help. Muslims are taught to be a “mirror” for each other and to encourage good behavior and discourage antisocial behavior (amr bil ma’roof wal nahyi ‘an al-munkar) in their community. If their advice fails, individuals are instructed to avoid the perpetrator so that he/she may turn back once they realize their ‘bad’ actions have resulted in their isolation (Dastghaib Shirazi, 1998). This moral worldview may also cause Muslims to underreport their own drinking. Muslims that drink still consider themselves sinners and Islam discourages confession or disclosing one’s sin to anyone (M. Ali, 2014). University or social-based interventions may need to be tailored for settings where alcohol is viewed from a moral (rather than medical) viewpoint. These may differ from approaches in non-MMCs (Stockings et al., 2016).
Considering that current mental health and substance treatment infrastructure is limited; contextual measures should be in place to prevent alcohol misuse in Iraq. This may help prevent an increase in the prevalence of drinking and associated risk behaviors as observed in other post-conflict MMC settings. For example, risk behaviors such as drink driving, carrying weapons, and physical fights associated with drinking are high in post-conflict Kirkuk and Erbil (Saeed, 2016; Shabila et al., 2015). Figures from Lebanon also show an increase in alcohol abuse (DSM-III & DSM-IV) by Muslim university students within eight years after the end of the civil war (increasing from 3.8% to 6.1%, from 1991 to 1999) (E. G. Karam et al., 2004).
To prevent alcohol misuse and associated risky behaviors, a consistent and strong alcohol policy is needed in Iraq. Participants in our study reported a diversity of opinions on policy approaches. Currently, Iraq has a mix of these policies on a federal, provincial, and local level (Al Ansari et al., 2019). For example, federally, alcohol sellers must be non-Muslim however, a consumer can be of any faith. However, in some provinces, alcohol sales and drinking are totally prohibited (e.g., Basra), and in others they are prohibited in certain areas (e.g., Kadhimiyya in Baghdad). Consistent with previous evidence (Stockings et al., 2016), our findings did not indicate that local prohibition impacts upon reported drinking prevalence or access to alcohol (compared to sites with no alcohol prohibition). Further details of this analysis have been with-held to avoid identifying participating universities. These policies may be compromised by weak law enforcement including a lack of policing at provincial borders.
In addition to strong border control, taxation is known to be the single most impactful preventative intervention in non-MMCs (T. Babor, 2010; Stockings et al., 2016). Iraq, however, does not have a digitized tax system and has limited ability to implement import or sales tax on specific commodities such as alcohol (International Monetary Fund, 2017). Monitoring, controlling, and taxing alcohol will prove difficult in the current volatile political and economic situation.
Students suggested that advice, warning, or education would be their preferred method of responding to someone who is caught with alcohol on their person. Given the mixed perceived motives for the uptake of drinking, this advice could be provided by parents, religious and cultural leaders, or medical professionals. Such advice could constitute brief interventions or evidence-based approaches to encourage those already using alcohol in an ‘at-risk’ way to re-think their drinking. The introduction of brief interventions in primary health settings may help to address harmful drinking. There is currently an initiative in Iraq to integrate mental health care into primary health care to ease the associated stigma of seeking such care in specialized facilities (Sadik, Abdulrahman, Bradley, & Jenkins, 2011). This is key given that trauma is the second highest perceived motive of drinking and that two fifths reported direct experience of war or violent military conflict. However, mental health is stigmatized in Iraq (Bolton, 2013). In addition, most young people are less likely to visit a medical practitioner to discuss alcohol use (Humphreys, 2011). The Iraqi health system is struggling to integrate mental health care into primary health care (Sadik et al., 2011). Additionally patient confidentiality is limited as primary health care practitioners rarely consult in private in Iraqi health settings (Al Ansari et al., 2019).
Information alone has been shown to be ineffective in curbing alcohol use and misuse, however, programs such as the positive youth development programs (PYDP) or family skill-based interventions have shown some promising results in curbing alcohol and other drug use (Stockings et al., 2016). These types of programs equip young people or their parents with psychosocial skills focusing on resilience, communication, and development without necessarily addressing alcohol exclusively. Given that religious, sociocultural, and family reasons are the main motives for abstinence and that drinking is associated with being non-Muslim and living away from family, in the absence of these protective factors, young people may be vulnerable to alcohol use and misuse. Globalization has led to increasing exposure to alcohol advertisements on the internet, social media, and satellite TV. Iraq’s alcohol policy should therefore be cognizant of this changing contemporary landscape to safeguard the growing Iraqi youth population into the future. This policy should take into consideration Iraq’s diverse populace, cultures, and religions as well as evidence-based approaches, locally sourced or adapted from other MMC and non-MMC experiences.
Limitations
The study sample could not be randomly selected due to the lack of student email databases within universities. Most collaboration and recruitment occurred within the medical faculties. During visits to other colleges, we were informed by staff that the use of internet for educational purposes was relatively new except in faculties such as Medicine, Engineering, and Pharmacy. This may have contributed to limited access from students of other faculties. Because of lack of external funding for this research, active recruitment at each site only lasted a few days while we were interviewing for the qualitative component of this study. Funding for further active recruitment could have increased the sample size.
While 448 people (86% of eligible participants) completed the substance use section, less than half (43.4%) completed the entire survey. We assume that this was because of the survey length (~15–20 minutes) as no association was observed between drinking patterns and the dropout rate. The largest dropout rate was found in validation questions that explore similarly concepts in questions with deliberately reversed phrasing (e.g., motives for drinking). Accordingly, future studies should be shorter and avoid any perception of repetition. An alternative explanation is that the topic of the survey (alcohol and drugs) caused offence. There were also some internal contradictions in some sensitive questions. For example, some people said they have had alcohol in the past 12 months and then then answered “never” to the first question of the AUDIT (about frequency of drinking in the last year). This could be because people who do not see themselves as “usual” drinkers answer “never”. As the PC-PTSD screen and the exposure to war question were placed toward the end of the survey, less than half of drinkers answered this question – so no conclusions can be drawn about alcohol use and war exposure. The survey did not enquire about other mental health conditions such as depression and anxiety. This could be an area for future study.
Conclusion
The prevalence of self-reported drinking in Iraq is consistently lower than countries in the developed world or non-MMCs. However, this study and others have indicated that drinking occurs at risky levels among many drinkers in this setting. A decline in abstention may lead to an increase in alcohol-related harm. Iraq’s healthcare system is ill equipped to cope with such an increase and to implement evidence-based preventive approaches. This reflects an ongoing need to accurately and regularly measure alcohol use using appropriate tested and tailored tools.
Innovative, low-cost, evidence-based approaches are required to prevent alcohol-related harms including skills-based youth and parental development programs. These initiatives should be tailored to and evaluated in the local settings. In addition, a clear and implementable alcohol policy that considers Iraq’s majority youth population and their experiences is needed.
Acknowledgement
We would like to thank Dr Michael Livingston for assisting us in devising and reviewing the survey. We would also like to thank Dr James Conigrave for advice on quantitative analysis for this study. A special gratitude also goes towards those who contributed to easing the way for this research to be undertaken in Iraq. Namely, we would like to thank Dr Jawad al-Diwan and Dr Wisam al-Lami for their time in assisting us with recruitment. We would also like to thank all students who contributed to promoting this survey, and in particular, Hussain al-Shadidi (IFMSA-Iraq) and Shams al-Niaimi, and finally, all those students who participated in the survey.
Notes
Conflicts of interest: The authors have no conflicts of interest to disclose.
References
Al-Ameri, R. J. K., Al-Badri, H. J. A., & Lafta, R. K. (2016). Prevalence of Alcohol Consumption among University Students in Baghdad: A Crosssection survey from Iraq. Epidemiology Biostatistics and Public Health, 13(4), e11942-11941–11948. doi:10.2427/1194210.2427/11942
Al-Ansari, B., Thow, A. M., Day, C. A., & Conigrave, K. M. (2016). Extent of alcohol prohibition in civil policy in Muslim majority countries: the impact of globalization. Addiction (Abingdon, England), 111(10), 1703–1713. https://doi.org/10.1111/add.13159https://doi.org/10.1111/add.13159
Al-Diwan, J., Al-Hemiary, N., & Hashim, M. (2015). Alcohol and Drug Abuse in Post-conflict Iraq. European Psychiatry, 30, Supplement 1(0), 1394. doi:10.1016/S0924-9338(15)31080-410.1016/S0924-9338(15)31080-4
Al-Hasnawi, S. (2006). Attitude of Residents and General Practitioners Toward Substance Abuse in Iraq. Medical Journal of Babylon, 3(1–2), 107–112.
Al-Hasnawi, S., Al-Hemiary, N., & Lafta, M. (2007). Public Attitudes toward Substance Abuse. Karbala Medical Journal, 1(2), 162–166.
Al-Hemiary, N., Hashim, M., Al-Diwan, J., & Abdul Razzaq, E. (2015). Alcohol and Drug Abuse in Post-Conflict Iraq. Journal of the Faculty of Medicine, Baghdad, 57(4), 290–294. doi:10.32007/jfacmedbagdad.57439210.32007/jfacmedbagdad.574392
Al-Hemiary, N. J., Al-Diwan, J. K., Hasson, A. L., & Rawson, R. A. (2014). Drug and Alcohol Use in Iraq: Findings of the Inaugural Iraqi Community Epidemiological Workgroup. Substance Use & Misuse, 49(13), 1759–1763. doi:10.3109/10826084.2014.91363310.3109/10826084.2014.913633
Al-Imam, A., Al-Mukhtar, F., Shafiq, A., & Irfan, M. (2017). Knowledge and (Ab) Use in Connection with Novel Psychoactive Substances: A Cross-Sectional Analysis of Iraqi Medical Students. Global Journal of Health Science, 9(11), 61. doi:10.5539/gjhs.v9n11p6110.5539/gjhs.v9n11p61
Al Ansari, M., Dawson, A., & Conigrave, K. (2019). Alcohol: from Mesopotamia to Modern Iraq. Journal of Ethnicity in Substance Abuse, 1–23. doi:10.1080/15332640.2019.165754110.1080/15332640.2019.1657541
Al Ansari, M., Dawson, A., & Conigrave, K. (2022). Alcohol among young people in Iraq: a systematic scoping review. Discover Psychology, 2(1), 16. doi:10.1007/s44202-022-00024-810.1007/s44202-022-00024-8
Al Mousawi, A. (2015). Alcohol use disorder identification test use in Muslim countries. International Journal of Prevention and Treatment of Substance Use Disorders, 1(3–4), 79–92. doi:10.4038/ijptsud.v1i3-4.784010.4038/ijptsud.v1i3-4.7840
Alcohol Public Policy Group. (2010). Alcohol: No Ordinary Commodity – a summary of the second edition. Addiction, 105(5), 769–779. doi:10.1111/j.1360-0443.2010.02945.x10.1111/j.1360-0443.2010.02945.x
Ali, M. (2014). Perspectives on Drug Addiction in Islamic History and Theology. Religions, 5(3), 912–928. doi:10.3390/rel503091210.3390/rel5030912
Ali, S., & Sabir, J. (2009). Prevalence of Alcohol Use among Medical College Students in Hawler Medical University. Zanko Journal of Medical Sciences, 13(1), 17–23. doi:10.15218/zjms.2009.00410.15218/zjms.2009.004
Australian Institute of Health and Welfare. (2013). National Drug Strategy Household Survey. Retrieved from Canberra: https://www.aihw.gov.au/reports/illicit-use-of-drugs/2013-ndshs-detailed/summaryhttps://www.aihw.gov.au/reports/illicit-use-of-drugs/2013-ndshs-detailed/summary
Babor, T. (2010). Alcohol: No Ordinary Commodity: Research and Public Policy. Oxford: Oxford University Press.
Babor, T. F., Higgins-Biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva: World Health Organization.
Baron-Epel, O., Bord, S., Elias, W., Zarecki, C., Shiftan, Y., & Gesser-Edelsburg, A. (2015). Alcohol Consumption Among Arabs in Israel: A Qualitative Study. Substance Use & Misuse, 50(2), 268–273. doi:10.3109/10826084.2014.96205110.3109/10826084.2014.962051
Bolton, P. (2013). Mental health in Iraq: issues and challenges. The Lancet, 381(9870), 879–881. doi:10.1016/S0140-6736(13)60637-610.1016/S0140-6736(13)60637-6
Bradley, K. A., McDonell, M. B., Bush, K., Kivlahan, D. R., Diehr, P., & Fihn, S. D. (1998). The AUDIT Alcohol Consumption Questions: Reliability, Validity, and Responsiveness to Change in Older Male Primary Care Patients. Alcoholism: Clinical and Experimental Research, 22(8), 1842–1849. doi:10.1111/j.1530-0277.1998.tb03991.x10.1111/j.1530-0277.1998.tb03991.x
Bullock, S. (2004). Alcohol, Drugs and student lifestyle: a study of the attitudes, beliefs and use of Alcohol and Drugs among Swedish University students: Centrum för socialvetenskaplig alkohol-och drogforskning (SoRAD).
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med, 158(16), 1789–1795. doi:10.1001/archinte.158.16.17810.1001/archinte.158.16.178
Dastghaib Shirazi, S. A. H. (1998). Greater Sins (Rizvi, S. A. H. S. H., Trans. Vol. 1). Mumbai: Islamic Study Circle.
GBD 2016 Risk Factors Collaborators. (2017). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 390(10100), 1345–1422. doi:10.1016/S0140-6736(17)32366-810.1016/S0140-6736(17)32366-8
Ghandour, L., Chalak, A., El-Aily, A., Yassin, N., Nakkash, R., Tauk, M., … Afifi, R. (2016). Alcohol consumption in the Arab region: What do we know, why does it matter, and what are the policy implications for youth harm reduction? International Journal of Drug Policy, 28, 10–33. doi:10.1016/j.drugpo.2015.09.01310.1016/j.drugpo.2015.09.013
Hamdieh, M., Motalebi, N., Asheri, H., & Boroujerdi, A. (2008). Prevalence of Alcohol and Drug Abuse in Young People, 15–35 Year Old, Living in Tehran, Iran. Pejouhesh, 32(4), 315–319.
Humphreys, K. (2011) Circles of Recovery: An Interview with Keith Humphreys, PhD/Interviewer: W. White. Counselor (Vol 12(6)).
International Monetary Fund. (2017). Iraq: Selected Issues (IMF Country Report No. 17/252). Retrieved from Washington D.C.: https://www.imf.org/-/media/Files/Publications/CR/2017/cr17252.ashxhttps://www.imf.org/-/media/Files/Publications/CR/2017/cr17252.ashx
Islam, M. M., Topp, L., Conigrave, K. M., van Beek, I., Maher, L., White, A., … Day, C. A. (2012). The reliability of sensitive information provided by injecting drug users in a clinical setting: Clinician-administered versus audio computer-assisted self-interviewing (ACASI). AIDS Care, 24(12), 1496–1503. doi:10.1080/09540121.2012.66388610.1080/09540121.2012.663886
Karam, E., Kypri, K., & Salamoun, M. (2007). Alcohol use among college students: an international perspective. Curr Opin Psychiatry, 20(3), 213–221. doi:10.1097/YCO.0b013e3280fa836c10.1097/YCO.0b013e3280fa836c
Karam, E. G., Maalouf, W. E., & Ghandour, L. A. (2004). Alcohol use among university students in Lebanon: prevalence, trends and covariates: The IDRAC University Substance Use Monitoring Study (1991 and 1999). Drug and Alcohol Dependence, 76(3), 273–286. doi:10.1016/j.drugalcdep.2004.06.00310.1016/j.drugalcdep.2004.06.003
Kelly, T. M., Donovan, J. E., Chung, T., Bukstein, O. G., & Cornelius, J. R. (2009). Brief screens for detecting alcohol use disorder among 18–20 year old young adults in emergency departments: Comparing AUDIT-C, CRAFFT, RAPS4-QF, FAST, RUFT-Cut, and DSM-IV 2-Item Scale. Addictive Behaviors, 34(8), 668–674. doi:10.1016/j.addbeh.2009.03.03810.1016/j.addbeh.2009.03.038
Lewis, M. A., & Neighbors, C. (2006). Social norms approaches using descriptive drinking norms education: A review of the research on personalized normative feedback. Journal of American College Health, 54(4), 213–218. doi:10.3200/JACH.54.4.213-21810.3200/JACH.54.4.213-218
Prins, A., Ouimette, P., Kimerling, R., Cameron, R. P., Hugelshofer, D. S., Shaw-Hegwer, J., … Sheikh, J. I. (2003). The primary care PTSD screen (PC-PTSD): development and operating characteristics. Primary Care Psychiatry, 9(1), 9–14. doi:10.1185/13552570312500236010.1185/135525703125002360
Ridout, B., & Campbell, A. (2014). Using Facebook to deliver a social norm intervention to reduce problem drinking at university. Drug and Alcohol Review, 33(6), 667–673. doi:10.1111/dar.1214110.1111/dar.12141
Sadik, S., Abdulrahman, S., Bradley, M., & Jenkins, R. (2011). Integrating mental health into primary health care in Iraq. Mental health in family medicine, 8(1), 39–49.
Saeed, H. M. (2016). Assessment of the Health Risk Behavior in Young Adulthood: A school-based Health Study in Kirkuk City/Iraq. Tikrit Medical Journal, 21(2), 172–181.
Shabila, N. P., Ismail, K. H., Saleh, A. M., & Al-Hadithi, T. S. (2015). Risky Driving Behaviours among Medical Students in Erbil, Iraq. Sultan Qaboos University Medical Journal, 15(3), e390–e397. doi:10.18295/squmj.2015.15.03.01410.18295/squmj.2015.15.03.014
Ṣirāmī, Ḥ., Qurbānī, M., & Mīnūnī, M. (2013). Barrisi Chahār dah Taḥqīqāt Shuyūʿ Shināsī Iʿtiyād dar Īrān [Review of 14 Prevalence Studies of Addiction in Iran]. Quarterly Journal of Research on Addiction, 7(26), 29–52.
Stockings, E., Hall, W. D., Lynskey, M., Morley, K. I., Reavley, N., Strang, J., … Degenhardt, L. (2016). Prevention, early intervention, harm reduction, and treatment of substance use in young people. The Lancet Psychiatry, 3(3), 280–296. doi:10.1016/S2215-0366(16)00002-X10.1016/S2215-0366(16)00002-X
UNDESA. (2017). World Population Prospects: The 2017 Revision, Key Findings and Advance Tables. Retrieved from https://population.un.org/wpp/publications/files/wpp2017_keyfindings.pdfhttps://population.un.org/wpp/publications/files/wpp2017_keyfindings.pdf
US Department of State, Bureau of International Narcotics and Law Enforcement Affairs, Iraqi Society of Addiction Medicine, University of California LA, & Center for Human Services. (2015). Survey of Substance Abuse in Iraq. Bethesda, MD.
WHO. (2006a). Interpersonal Violence and Alcohol. Retrieved from Geneva: http://www.who.int/violence_injury_prevention/violence/world_report/factsheets/pb_violencealcohol.pdf?ua=1http://www.who.int/violence_injury_prevention/violence/world_report/factsheets/pb_violencealcohol.pdf?ua=1
WHO. (2006b). Public health problems of alcohol consumption in the Region. Retrieved from https://apps.who.int/iris/handle/10665/122425https://apps.who.int/iris/handle/10665/122425
WHO. (2009). Iraq Mental Health Survey 2006/7. Baghdad: World Health Organization.
WHO. (2010). ATLAS of Substance Use Disorders. Country Profile: Iraq. Retrieved from http://www.who.int/substance_abuse/publications/atlas_report/profiles/iraq.pdfhttp://www.who.int/substance_abuse/publications/atlas_report/profiles/iraq.pdf
WHO. (2014). Global Status Report on Alcohol and Health. Retrieved from Geneva: http://www.webcitation.org/6mk3vWQQmhttp://www.webcitation.org/6mk3vWQQm
Yazbek, J.-C., Haddad, R., Bou Khalil, R., Hlais, S., Rizk, G. A., Rohayem, J., & Richa, S. (2014). Prevalence and Correlates of Alcohol Abuse and Dependence in Lebanon: Results from the Lebanese Epidemiologic Survey on Alcohol (LESA). Journal of Addictive Diseases, 33(3), 221–233. doi:10.1080/10550887.2014.95002610.1080/10550887.2014.950026