Introduction
In recent decades, Muslims and Islam have been subject to increased scrutiny in Australia, as is the case in other Western nations (Bloemraad et al., 2008; Poynting & Mason, 2006, Yasmeen, 2016). Contemporary issues associated with Muslims, such as international terrorist attacks and asylum seekers fleeing to the West, have continued to drive a mixture of both interest and fear about Muslims and the religion of Islam (Aly, 2010; Morgan & Poynting, 2012; Poynting & Mason, 2007; Yasmeen, 2016). Yet, there has been relatively limited research in Australia regarding Muslims’ perspectives and experiences of seeking help for mental health problems; despite the fact that Australian Muslims face a range of stressors and inequalities within Australian society, which represent risk factors for mental health problems (Dunn et al., 2004; HREOC, 2004; IWWCV, 2008; Kalek et al., 2010; Khawaja, 2007; WHO, 2012). Some of these stressors include discrimination, stigmatization, social isolation, threats to identity, substantive cultural adjustment, and lower socio-economic status (Dunn et al., 2004; HREOC, 2004; IWWCV, 2008; Kalek et al., 2010; Khawaja, 2007; WHO, 2012). Research is required to understand of the barriers and facilitators for Muslims seeking mental health treatment.
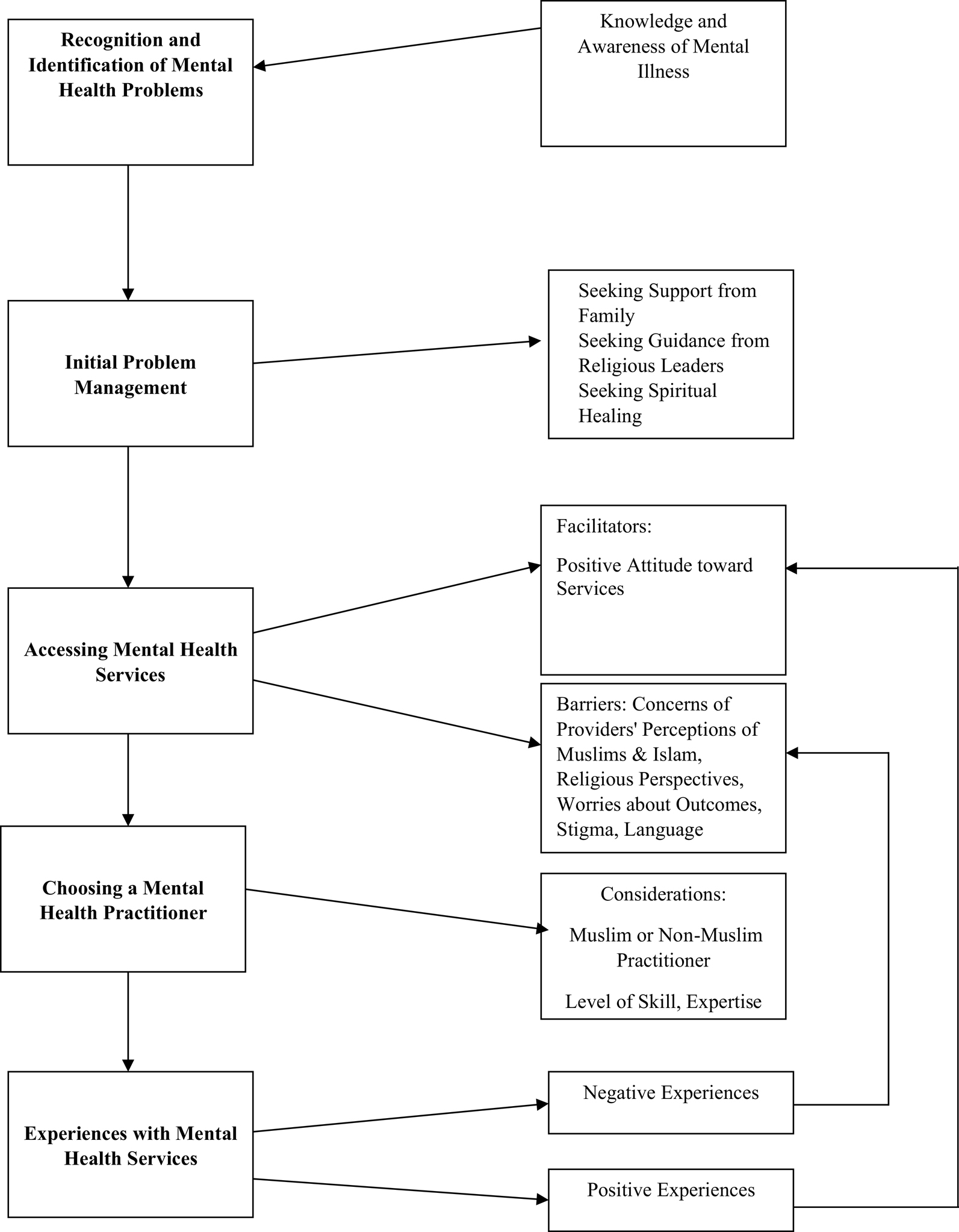
This article seeks to present a model of help-seeking behaviors based on in-depth interviews and survey data of Australian Muslims and their perspectives and experiences of seeking mental health treatment. The model demonstrates that Australian Muslims pass through various stages before seeking professional mental health treatment, including attitudinal barriers and stigma associated with seeking mental health services. The model shows that informal sources of support, such as religious leaders, are often sought before accessing formal mental health services. Once formal mental health services are accessed, the nature of the experience, whether positive or negative, will determine whether the attitudes towards mental health services are changed. This model provides a way to conceptualize the process of seeking professional mental health services for Australian Muslims.
Literature Review
The available research indicates that there are a range of attitudinal barriers in terms of accessing mental health services for Muslims residing in both majority-Muslim and minority-Muslim societies. Al-Darmaki (2003) examined the attitudes of 350 Emirati Arab undergraduate students by administering the measure of Attitudes Toward Seeking Professional Help (Fischer & Turner, 1970). The students identified various barriers to help-seeking, including a perception of stigma, fear of treatment, and reluctance to self-disclose. An important limitation with this study was that the participants were unable to elaborate on their views of these barriers and whether they may be open to change. Research involving Muslims living in Western countries also suggests attitudinal barriers to accessing professional mental health treatment. Weatherhead and Daiches (2010) identified several issues relating to Muslims’ help-seeking in the United Kingdom. Although participants expressed positive perceptions of professional treatment, help-seeking barriers included fears of stigma, negative stereotyping, and previous negative experiences with services. Participants emphasized the importance of practitioners providing religiously and culturally sensitive treatment. Although this study provides valuable findings, it offers limited exploration of the meaning of these barriers for participants, such as the ways in which the barriers were developed or reinforced, the extent that they prevented access to mental health services, and ways that they could be challenged.
There has been some research that investigates the attitudes of Muslims residing in the United States towards accessing mental health services. Khan (2006) investigated the attitudes of Muslims living in Ohio toward help-seeking, as well as the need for and use of professional counseling services. A total of 459 Muslim participants completed the Attitudes Toward Seeking Professional Psychological Help Scale (Fischer & Turner, 1970). Like other investigations (Weatherhead & Daiches, 2010), Khan (2006) found that the participants reported a need for mental health assistance. Despite most respondents holding positive attitudes towards counseling, there was a lack of usage of mental health services. The majority reported turning to alternative sources of help such as prayer, the Qur’an, and family. However, the study did not explain the limited uptake of services.
In another study conducted in the United States, Aloud and Rathur (2009) investigated attitudes towards accessing mental health services among 279 Arab Muslims. The participants completed the Attitudes Toward Seeking Professional Psychological Help Scale (Fischer & Turner, 1970) and two instruments developed for the research, the Cultural Beliefs About Mental Health Problems and Knowledge About and Familiarity with Formal Mental Health Services. Based upon their findings, Aloud and Rathur (2009) developed a model of help-seeking behaviors among Arab Muslims called the Help-Seeking Pathways of Arab Muslims (HSPAM). According to the HSPAM, Arab Muslims tend to go through three stages when experiencing mental health problems and encounter a range of personal, professional, and organizational obstacles when progressing through these stages. In the first stage, becoming aware and recognizing a problem, the model proposes that Arab Muslims may be influenced by cultural and religious conceptions of mental illness, individual knowledge of mental illness and its treatment, and Arab coping styles. In the second stage, deciding to seek help, the model indicates that social stigma associated with mental health problems, negative attitudes towards service providers, a lack of confidence in formal services and their providers, and the use of other supports such as family and community networks, may impede access to services. In the third stage, service selection, Arab Muslims’ help-seeking behaviors may be influenced by the preference for religious healing, a lack of awareness of available services, acculturation influences, and economic and institutional barriers. While Aloud and Rathur’s (2009) research provides a useful framework to understand the help-seeking patterns amongst a group of Arab Muslims, it is necessary to explore in some detail Muslims’ personal experiences of each of these stages. Gaining an understanding of such barriers to accessing services, how they developed, and the factors that maintain them may assist in determining ways that these issues can be effectively addressed within Muslim communities.
One of the few studies of help-seeking behaviors that includes Australian Muslims was performed by Youssef and Deane (2006). The researchers conducted semi-structured interviews with 35 Arabic-speaking participants (including Muslims and Christians), exploring their perceptions of mental illness in the Arab community and their preferred forms of support and treatment. In terms of help-seeking, the participants identified religious leaders as a first point of contact for mental health problems. As far as treatment was concerned, most participants (91%) considered that their community would usually turn to spiritual healing or religious practices. The study also found that there was a lack of knowledge about available services. A key limitation of this study is that no distinctions were made between the perspectives of the Muslim and Christian participants. Furthermore, there are many non-Arabic speaking Australian Muslims, and therefore research is required to determine the factors that influence help-seeking for other cultural and linguistic groups.
Other studies in the United States have highlighted the position of imams for the Muslim community in responding to personal issues. Abu-Ras et al. (2008) investigated the role of 22 imams from mosques in New York City regarding mental health promotion. The imams completed a survey specifically designed for the research to elicit information regarding the mental health needs of the Muslim community since September 11 and their role in addressing those needs. The study found that the imam was usually the first and only contact for the worshippers’ personal and mental health problems, and yet most imams were not knowledgeable about mental health resources in the community. Although research identifies the significant position of religious leaders for Muslims (Abu-Ras et al., 2008; Osman, et al., 2005), investigation is needed to further understand their role in meeting Muslims’ mental health needs.
The evident role of religion in Muslims’ support-seeking behaviors indicates a need to examine the cultural competence of services provided for Muslims. Interest in culturally competent approaches has been driven by research that shows large inequities in access and quality of mental health care offered to minority groups (Mallinger & Lamberti, 2010). Practitioners are increasingly acknowledging the need for mental health services to provide culturally competent care and treatment (Geerlings et al., 2017, Hsieh & Bean, 2014; Huey et al., 2014). Research indicates that religiously and culturally competent treatment can improve engagement with mental health services and improve treatment outcomes. For example, Ribeiro and Saleem (2010) created an outreach group to address the observation that Muslim college women underutilize university counseling centers due to discrimination and negative stereotyping. The outreach group provided an opportunity for participants to explore a range of relevant issues impacting their lives. The participants provided positive feedback about the outreach group and all the women reported that they would continue to attend if a non-Muslim, but culturally sensitive, person led the group. Such findings suggest that awareness of the needs of minority and culturally diverse clients may increase services utilization.
Research by Graham et al. (2008) highlights the effectiveness of providing culturally sensitive service to clients. This study conducted interviews with 50 Canadian Muslim and non-Muslim practitioners working with Muslim clients. The research identified relevant cultural and social considerations for culturally sensitive treatment when working with Muslims. Some of these considerations included awareness of the roles of kinship, faith, and gender issues among Muslims, in addition to Muslims’ perceptions of counseling and pathways to care. Social issues, including relocation, isolation, institutional challenges, and racism, were also relevant to understanding the challenges faced by Muslims living in a majority non-Muslim society.
The current literature (Abu-Ras et al., 2008; Al-Krenawi, 2002; Al-Krenawi & Graham, 2000; Aloud & Rathur, 2009; Ciftci et al., 2013; Farooqi, 2006; Graham et al., 2008; Keshavarzi & Haque, 2013; Kira et al., 2014; Tanhan & Francisco, 2019; Weatherhead & Daiches, 2010) shows that there are a range of barriers in accessing mental health services for Muslims in both majority-Muslim and minority-Muslim societies, such as stigma, negative attitudes towards service providers, a preference for religious healing, and a preference for seeking help from family and religious leaders. However, the precise pathways of seeking mental health assistance for Australian Muslims is relatively un-researched. Therefore, this research aims to investigate Australian Muslims’ experiences and perspectives of seeking help for mental health problems through in-depth, face-to-face interviews and an online survey. Mixed methods approach provides advantages of offsetting the weakness of one type of data and expands the understanding of attitudes in help-seeking behaviors. Grounded theory was used for data analysis and development of a model to explain Muslims’ help-seeking.
Method
The limited research, coupled with reports that Australian Muslims consider that Islam and Muslims are generally misunderstood by the broader community (Dunn et al., 2015; Hopkins, 2011; HREOC, 2004), indicates that qualitative research is needed to gain deeper insights into the lives of Muslims and their perspectives and experiences of mental illness. Qualitative methods can offer a rich source of data to understand areas of commonalities and convergences (Thyer, 2010). This research employed face-to-face, in-depth interviews, which was followed by an online survey to investigate Australian Muslims’ perspectives and experiences of mental illness and mental health services. Grounded theory was utilized to analyze the data and develop the final model.
Procedure
Appropriate ethics approval was obtained prior to conducting the research. Participants were recruited for the in-depth, face-to-face interviews. The data gained from the interviews were used to inform the development of the survey, which was circulated among Australian Muslims online. Grounded theory was used to identify key themes from the interviews and comments sections of the survey to develop the model of help-seeking.
Interview Participant Recruitment
To recruit participants from a diverse range of backgrounds, several Islamic organizations were approached in Melbourne, including Islamic community centers (N = 2), mosques (N = 4), an Islamic school (N = 1), religious study groups (N =3), and a Muslims’ Arabic language study group (N = 1). At each organization, the researcher discussed the project with both groups and individuals and extended an invitation for participants. The criteria for this study were that potential participants were 18 years or above, residing permanently in Australia, and considered themselves to be a “practising Muslim.” No objective criteria were applied to being a practising Muslim. The notion of a “practising Muslim” can mean different things to different people and tends to be a subjective appraisal (Abu-Ras & Hosein, 2015). It was therefore considered appropriate that this was determined by the participants. It was not a requirement to have previous experience with mental health issues or treatment services; rather their views, perceptions, and attitudes were sought regardless of their prior knowledge of mental illness or experience with mental health services. Recruitment continued until the researcher had included participants who represented a range of cultural, educational, linguistic, and educational backgrounds. The participant characteristics were documented throughout the research process.
Interview Participant Sample
For the face-to-face interviews, 20 Australian Muslims were interviewed, consisting of 10 males and 10 females ranging 22–50 years of age (M = 32.70; SD = 9.69). The participants represented a range of cultural and linguistic backgrounds, including Lebanese (N = 7), Turkish (N = 1), Albanian (N = 1), Eritrean (N =1), Senegalese (N = 2), Pakistani (N = 2), Egyptian (N = 2), Palestinian (N = 1), Chinese (N = 1), and Australian Anglo-Saxon (N = 2). Most of the participants (N = 17) were born into Muslim families, with three being converts to Islam. The participants who had converted were between 16–24 years of age at the time they had converted. Most of the participants (N = 15) were born and raised in Australia, while five were born overseas and migrated to Australia as adults. The participants were given gender and culturally appropriate pseudonyms to maintain anonymity while highlighting their distinctive voices and assisting the reader to envision them in their world (Charmaz, 2006; Saldana, 2011).
Interview Participants: Pseudonyms and Descriptions
Participant |
Sex |
Age at Interview (years) |
Experience with Mental Health Services (Y/N) |
|---|---|---|---|
Hanan |
Female |
30 |
Y |
Nadia |
Female |
32 |
Y |
Amin |
Male |
42 |
N |
Rayann |
Female |
28 |
N |
Tasneem |
Female |
25 |
N |
Kareema |
Female |
36 |
N |
Layla |
Female |
28 |
Y |
Rana |
Female |
40 |
Y |
Amira |
Female |
24 |
Y |
Zaid |
Male |
22 |
N |
Ali |
Male |
19 |
N |
Marwan |
Male |
41 |
N |
Sameera |
Female |
45 |
Y |
Amir |
Male |
52 |
N |
Imran |
Male |
38 |
Y |
Adnan |
Male |
23 |
N |
Bilal |
Male |
35 |
N |
Hidaya |
Female |
22 |
N |
Mahmoud |
Male |
24 |
N |
Umar |
Male |
48 |
N |
Interview Procedure
The interviews were conducted in a range of settings, selected based on convenience and comfort for the participants, between June and December of 2014. These settings were in the participants’ homes (N =12), in an office at the participants’ place of work (N =5), in a café (N = 2), and in an Islamic center (N = 1). In all the settings, the interviews were conducted either in a separate room or in an area away from others for privacy. The duration of each interview was approximately one hour.
Interview Questions
In seeking to understand Muslim’s perspective on mental health and help-seeking behaviors, the central question was: “What are the perceptions and experiences of Muslims in regard to their mental health and accessing treatment services?” This question was deliberately broad to maintain an open perspective to the phenomena under investigation (Glaser, 1978, 1992; Strauss & Corbin, 1990, 1998). This stance of openness is consistent with the grounded theory methodology and allows the direction of the research to be guided by what is important to the participants. As the research progressed, a range of more specific questions related to the focus of the research was formulated to guide the interviews. These questions were designed to prompt discussion and facilitate reflections from the participants regarding their perspectives on and experiences of mental health and illness, and use of treatment services. For example, “What are your experiences with mental health services?” and “What are the barriers or concerns in accessing mental health services both for you and in the Muslim community?” These questions were formulated through consultation with stakeholders within the Muslim community, who provided feedback on the wording and content. The interview schedule was used in a flexible way, allowing the participants to direct the course of the interaction and raise experiences or issues they considered to be important.
Online Survey: Development and Procedure
An online survey (Muslim Mental Health Survey) was used to target a broader sample of Australian Muslims. The survey was designed following the in-depth interviews to extend the qualitative data by further exploring themes that emerged from the face-to-face interviews. The survey was intended to gauge the participants’ perspectives, responses, and attitudes relating to specific ideas and experiences. As such, the individual items were the focus of analysis.
As no existing measure was available, the researcher developed this survey for the purposes of the research. The data from the face-to-face interviews with participants in Australia was used to guide the development of the items. The items sought to explore attitudes in the following six areas: prior experiences with services, views of counseling, services for Muslims, Muslims and mental health, community and religious support, and accessing services.
The survey included items relating to demographic information of the participants, which was followed by the series of items regarding their attitudes towards mental illness, coping, and seeking help for mental health problems. The final survey included 28 items. Some items (4) required a “Yes/No” response, a selection from a list of forced-choice options, or an open-ended response. Most of the items (24) were phrased as statements to gauge attitudes. These included the same 4-point Likert scale response options: 1=Strongly Agree, 2=Agree, 3=Disagree, and 4=Strongly Disagree. These options were used to ensure consistency in the response format throughout the survey (Groves et al., 2009; Krosnick & Presser, 2010). The space for comments following each item allowed for written reflections from respondents, which provided additional qualitative data for the development of concepts.
Procedure
The survey was piloted with five Australian Muslims. Pilot testing new surveys is necessary to ensure that questions are clear and identify items that reflect researcher bias (Punch, 2003). Several changes were made based upon the feedback, predominantly related to expressing the items more clearly. Once finalized, the survey was uploaded on the PsychData Surveys website and was available from January to December of 2016.
Survey Participant Recruitment
Participants were recruited through the distribution of information fliers. These were distributed at Islamic meetings and organizations in Melbourne, Perth, and Sydney, including an Islamic conference (N = 1), mosques (N = 4), Islamic study circle (N = 3), and Islamic community centers (N = 2). The information flier was also distributed electronically through two Australian Muslim email groups. The fliers invited respondents to participate in the survey and included information about the researcher, the aims and nature of the project, and provided a link to the survey.
Survey Participants
A total of 214 respondents completed the survey. Of these, 14 were excluded as they indicated that they were not practising Muslims.
Of the final sample, 49 were male and 151 were female. The demographic characteristics of the respondents are presented in Table 2. As indicated in Table 2, most of the participants (N = 166; 83%) were relatively young, being aged under 40 years. Of note, the Australian Muslim population is significantly younger than the Australian population; over 80% are aged 44 and under (compared to just over 60% of non-Muslim Australians). Only 3.4% of the Australian Muslim population is aged 65 years and over (Hassan, 2015). Although almost half of the participants were born in Australia, affiliations with over 75 different cultural backgrounds were identified, with representations from countries across the world including Africa, the Middle East, Asia, and Europe. This cultural diversity is reflective of national data (ABS, 2016). Throughout the discussion, the survey participants are referred to by number (for example, survey respondent 12).
Survey participant characteristics (N = 200)
Demographics |
N (%) |
|---|---|
Participants’ age in years |
|
18–29 |
106 (53.0%) |
30–39 |
60 (30.0%) |
40–49 |
18 (9.0%) |
50–59 |
8 (4.0%) |
60–69 |
4 (2.0%) |
70–79 |
1 (0.5%) |
80+ |
3 (1.5%) |
Educational Attainment |
|
Secondary Schooling |
18 (9.0%) |
Certificate |
14 (7.0%) |
Diploma |
24 (12.0%) |
Undergraduate/Bachelor |
90 (45.0%) |
Postgraduate degree |
47 (23.5%) |
Other |
7 (3.5%) |
Country of Birth |
|
Born in Australia |
94 (47.0%) |
Born overseas |
106 (53.0%) |
Religion |
|
Born Muslim |
164 (82.0%) |
Converted to Islam |
36 (18.0%) |
Qualitative Data Analysis: Interview Transcripts and Survey Data
Grounded theory methodology was used to analyze the qualitative data, including that from the interviews and further comments offered in the online survey. The data analysis was undertaken in three main steps, consisting of initial coding, focused coding, and theoretical coding. This process was not conducted in distinct stages, rather it involved moving back and forth between the data and the analysis to identify relationships between concepts.
Quantitative Data Analysis: Survey Data
For the survey data statistics, the quantitative data from the survey was entered into an Excel spreadsheet and then imported into the statistical analysis software, Statistical Package for Social Scientists (SPSS). Statistical analysis was performed on the individual items to determine percentages of participant agreement or disagreement with each item.
Results
Recognition and Identification of Mental Health Problems
Knowledge and Awareness of Mental Illness
When considering help-seeking for mental health problems, the participants identified that an essential first step is recognizing symptoms of mental illness (see Figure 1). Participants across the samples highlighted issues with recognizing mental health problems within their communities. They noted that a lack of identification may result in sufferers failing to seek help for treatable mental health conditions. Interview participant Zayd commented:
Participants acknowledged that raising awareness among the Australian Muslim community is necessary to increase identification of mental health conditions and thereby improve access to appropriate treatment. Concern about the awareness of mental illness in the Muslim community was confirmed by the survey participants. The overwhelming majority (N = 199; 99.5%) of respondents agreed that more information and education about mental health is needed for Muslim communities. The recognition of symptoms of a mental health problem was therefore seen as a necessary step in seeking help.… people might have a mental illness and someone just says that’s just how he is… . if we don’t know what the signs are of mental illness, we don’t know what the symptoms are and all those sorts of things then how do we know someone’s mentally ill? We could think that’s just how they are.
Initial Problem Management
Seeking Support From Family
The participants emphasized that in their communities, family support was a vital part of their problem management and help-seeking process (see Figure 1). Amin described the steps as first seeking help from family, then from the community, and then from the local sheikh. Amin commented:
In our community, the first thing we try to do is we try to solve our own problems, so the parents get involved if they can solve it. If not, someone else who is highly regarded in the community will try to get involved. When they can’t, they go to the sheikh.
Seeking Guidance From Religious Leaders
Across the samples, participants indicated a prominent role for religious leaders in assisting Muslims with personal concerns. The participants described religious leaders, such as an imam or sheikh, as being highly respected in their communities, and seeking their help was a way to gain religious perspectives and spiritual guidance to cope with personal difficulties. Despite the prominent role for religious leaders, the survey responses highlighted concerns about seeking their help for mental health difficulties. More than half of the survey respondents did not consider religious leaders to be an ideal source of help for mental health problems or have sufficient understanding of mental health. Related to this, survey respondent 4 indicated, “They do try to provide whatever support they can give but unfortunately, they have not been trained to do this. Whilst some may become good at it by experience, but this is widely lacking.” Overall, the participants saw a role for religious leaders in providing guidance and faith perspectives for personal problems. However, the survey respondents were concerned about religious leaders’ knowledge of mental health, and this limited the assistance that they could provide.
Seeking spiritual healing: The data revealed that it is common for psychological conditions to be attributed to supernatural causes such as black magic (sihr), spirits (jinn), or the evil eye (ayn) in the participants’ communities. As such, participants said that they preferred to be treated with spiritual healing from religious healers, such as an imam. This involved healing through Qur’anic verses, known as ruqi’ah. As shown in Figure 1, spiritual healing is a type of informal help used in the initial stages of problem management.
The survey respondents similarly drew attention to the use of spiritual treatment in the Muslim community. Survey respondent 183 said:
The participants indicated that seeking professional treatment tended to be a fraught decision. A range of complex considerations appeared to either facilitate, or inhibit, their access to mental health services.Counseling and medication might not be the answer for certain people, as the patient could be experiencing difficulties from demons [Jinns] or Shaitan [Satan]. In this situation, dua [supplication] and or ruqi’ah [Islamic healing] derived from the sunnah [way] of Prophet Muhammed would be advisable from Islamic scholars and imams.
Accessing Mental Health Services: Facilitators
Favorable Attitudes Towards Services
As depicted in Figure 1, a positive view of mental health services emerged as a key aspect in accessing mental health treatment. Such attitudes were particularly evident in the interview data. From the interviews, 19 of the 20 participants expressed favorable attitudes regarding the usefulness of professional mental health services. Interview participant Hanan reflected upon the benefits of mental health services, “I think it’s a great thing. If you have an issue and you don’t get the skills to deal with it, it’s going to go on forever.”
Due to the central role of religious beliefs and practices in participants’ lives, the compatibility of professional mental health treatment with their religion was a relevant consideration. According to both interview participants and survey respondents, their religious perspectives and practices could be complementary to mainstream models of mental illness and its treatment. For example, participants considered that beliefs in supernatural phenomena did not preclude a mainstream view of mental illness that included biological, psychological, and environmental causes. As such, there was an overlap between the participants’ religious beliefs and mainstream models of mental illness and treatments. In this regard, participants asserted that Islamic teachings encourage an openness to seeking help from other sources.
The survey results similarly provided positive perceptions of professional mental health treatment among Australian Muslims. From the survey respondents, 97.5% were of the view that counseling and psychological services can be beneficial for Muslims. Most respondents also disagreed that Muslims should deal with their problems within their communities without seeking help from professionals. Additionally, most respondents (N = 153; 76.5%) expressed a willingness to consider seeking help from a counselor or psychologist in the future.
The comments provided by survey respondents elaborated on the positive perceptions. For example, survey respondent 173 commented:
These comments reflect favorable views regarding a range of mental health services among Australian Muslims. Even so, it is noteworthy that close to 1 in 5 of the survey participants would not consider such help. Indeed, concerns about accessing mental health services were identified.Being healthy is strongly encouraged in Islam. Mental health is a very important aspect of health and being healthy means being mentally healthy as well, not only physically. With the increased rate of mental illness, it is important for Muslims to keep mentally healthy—even if it means through counseling.
Accessing Mental Health Services: Barriers
As depicted in Figure 1, a range of barriers to accessing mental health services were evident in the data. Some of the issues which emerged included shame and stigma about accessing treatment, concern about the cultural and religious appropriateness of treatment approaches, and fear about accessing treatment.
Stigma Associated with Mental Illness
Across the data, a common issue was the community stigma attached to mental illness, resulting in a sense of shame and reluctance to access treatment. Participants observed that in their communities, mental illness is often associated with being “crazy” and, therefore, people with mental illness are unable to manage their problems. As a result of this stigma, there were issues acknowledging mental health problems and accepting the need for treatment. The participants’ perceptions of the extent to which stigma is a problem in their communities varied. For 15 of the 20 Australian interview participants, stigma was seen to be problematic because it was attached not only to the individual requiring treatment but also to their families. This reluctance was highlighted by Ali when he stated, “I probably still have that misconception that going to see a counselor convinces you that you’re not a 100% … within this community we have this misconception that going to seek counseling services, that it must be a major issue.”
Regarding the survey data, although not pronounced, issues of stigma were evident. Most respondents (N = 163; 81.5%) disagreed that they would feel embarrassed about accessing services with a counselor or psychologist. In addition, most (over 80%) agreed that their family members would approve of them accessing mental health services. However, 50% of survey respondents were of the view that their family members would feel embarrassed to talk about their mental health difficulties with a professional. Such data indicates some inconsistency in the extent to which shame is attached to accessing professional help among the Australian Muslim community.
Concern Regarding Providers’ Perceptions of Muslims and Islam
A barrier that emerged from the data was concern about the provider’s ability to offer religiously and culturally appropriate treatment. A total of 13 of the 20 interview participants stated that they were concerned about mental health practitioners’ perception of practising Muslims. They commented that Islam and Muslims are viewed negatively in the broader Australian society. This was largely seen to occur because of the adverse media portrayal of local and international events involving Muslims, and public discussion regarding the incompatibility of Muslims living in Australian society. In this context, participants stated that they feared mental health service providers would view Muslims according to the same negative stereotypes. Interview participants Mahmoud commented, “The client’s going to keep thinking at the back of their mind, this person may be perceiving me as a terrorist. So, the client’s going to always be fighting that thought in their mind.”
Similar issues were evident from the survey data. Half of the respondents were of the view that non-Muslim counselors and psychologists do not have a good understanding of Muslims’ problems. Furthermore, 61% agreed that mental health practitioners can have biased or stereotypical attitudes towards Muslims. These concerns were noted in their comments. For example, respondent 23 stated, “Muslim counselors are aware of the boundaries and lifestyles in a Muslim’s life. Non-Muslims … may perceive our lifestyle as oppressive and encourage things that are not appropriate.”
Worries About the Treatment Process
Another barrier consisted of a range of worries regarding engaging with mental health services. Several participants feared that practitioners would steer them away from their religious beliefs and values. Over 60% of respondents were of the view that non-Muslim counselors or psychologists may encourage Muslims to adopt solutions which are against Islam. Other worries were raised by participants about engaging in treatment, regardless of whether the practitioner was a Muslim. Participants feared the use of medication and the prospect of hospitalization. Interview participant Rana shared her uncertainty before engaging in treatment with a psychologist, “Not knowing what was happening, how they were going to approach me, deal with my situation, if they were going to be fully understanding, if they were going to judge me for what I’ve been through, just not knowing how they’re going to take it.”
For some participants, the fears associated with mental health treatment resulted in them delaying or avoiding engagement with professional mental health services.
Religious Perspectives as Barriers to Treatment
Although participants highlighted the beneficial aspects of faith on their mental health and coping, some observed that an over-emphasis on certain religious beliefs could be counterproductive. These beliefs were, at times, propagated within the Muslim community through Islamic lectures and discussions. This included the notion that mental illness may be a result of a weakness of faith, which could be disheartening. Interview participant Rana shared about when she was referred to a psychologist for anxiety:
The participants recommended that there be a balance between religious and secular perspectives of mental illness. This would enable Muslims to draw on the beneficial aspects of their faith to cope while leaving them open to the possibility of accessing professional mental health treatment.My mum, first of all, pointed out that I have a lack of iman [faith] and that … really put me down a bit, my self-esteem. Then just having to realize that, alright, everyone has a different opinion but that’s not necessarily the right opinion, that I have to do what’s right for me.
Language as a Barrier
Lastly, participants observed that for migrants to Australia, difficulties with the English language can serve as a barrier to accessing mental health treatment. Interview participant Hanan referred to her mother’s difficulties migrating to Australia as an adult. Despite experiencing great distress, she had avoided accessing services. Hanan commented on how her mother couldn’t find mental health professionals who could speak her language and understand her experiences:
Interview participants Amir and Mahmoud explained that although they were reasonably fluent in spoken English, it was a struggle to express the nuances of their internal experience. Mahmoud observed that in overcoming such barriers, it was important to have psychologists who speak the language of the community. “To explain a mental problem, you’re going to have to be able to speak to that person in their language.” Such comments highlight a need for access to practitioners who are aware of religious and cultural issues, but also who speak the language of community members.My mum didn’t get help, because she was referred to the psychologist who don’t get that they’re married for almost forty years, and she’s had seven kids, her life has been tough, she’s illiterate, they don’t get where she came from, they don’t speak her language.
Choosing a Mental Health Practitioner
For both the interview participants and survey respondents, an issue was whether to seek assistance from either a Muslim or non-Muslim mental health practitioner (see Figure 1).
Preference for a Muslim Mental Health Practitioner
Generally, participants preferred to access services with a Muslim practitioner as they felt that their religious beliefs and practices would be understood. An advantage to seeking services with a Muslim practitioner was the expectation that relevant religious and cultural concepts would not need to be explained, which may be time consuming and disrupt the flow of counseling.
The views expressed by the interview participants in relation to accessing Muslim mental health practitioners were confirmed by the survey data. The data revealed that almost half (45%) of the respondents would only seek mental health services from a Muslim counselor/ or psychologist. As survey respondent 25 explained:
Like the interview participants, the survey respondents largely agreed (87%; N = 174) that more Muslim mental health practitioners were needed to support the Australian Muslim community.I believe practising Muslim professionals have a better understanding of the context in which Muslims live and their day-to-day problems. Therefore, a Muslim practitioner could be of more benefit to the patient. Also, if the professional is knowledgeable about Islam, they can offer Islamic remedies for mental illnesses and personal problems they may be suffering.
Preference for a Non-Muslim Mental Health Practitioner
Along with the advantages, a range of disadvantages were identified in accessing assistance from a Muslim mental health practitioner. These included a fear of contact outside the context of treatment due to the relatively small size of the Muslim community in Australia. These concerns were evident in the survey data. Survey respondent 127 commented on weighing the advantages between shared beliefs with the practitioner and their level of skill and experience:
For some respondents, religious affiliation was not a consideration in seeking treatment, such as survey respondent 42, who said, “As long as the counselor is capable of providing the services, I don’t think religion matters that much.” The survey data revealed that for Muslims deciding to access professional treatment, there are a range of issues that have the potential to complicate the help-seeking process. Accessing treatment from a Muslim practitioner was generally preferred, however this option raised concerns for the participants.I think it’s human nature to feel more comfortable with people that have similar perspectives or hold similar views, having a Muslim counselor would be beneficial in that they can assist a patient with offering them advice based on their similar experiences and can relate to them more.
Experiences with Mental Health Services
The previous experience of participants with mental health services had a profound impact on their attitudes towards accessing services in the future.
Positive Experiences
Positive treatment experiences left a favorable perception of mental health professionals, which reinforced facilitators to accessing mental health services (as shown in Figure 1). This included the practitioner adopting a stance of respect for the participants’ beliefs and practices, being aware of the significance of religion and culture in their lives, and showing an interest in the way religion related to their problems and possible solutions.
Survey respondent 164 described feeling comfortable exploring her religious issues and concerns with a Muslim practitioner:
Such comments emphasize the benefits of religious and cultural awareness, particularly in overcoming barriers for Muslims in attending mental health services.Initially, I felt it would make no difference. But when I went to a Muslim counselor, I felt more comfortable as I could explain things better to her, how I felt regarding my level/state of iman [faith]. She even suggested [to] me ways on how to get regular with my prayers.
Negative Experiences
Participants also identified negative experiences that reinforced barriers to accessing mental health treatment (as depicted in Figure 1). These included a lack of practitioner awareness of relevant cultural and religious issues, as well as deferring to stereotypes. The participants considered that a lack of understanding of religious and cultural issues had a negative impact upon the effectiveness of the services. Survey respondent 27 shared her experience with counseling:
Negative treatment experiences left a lasting impression on the respondents. Participants mentioned they were careful about the personal information they disclosed to the practitioner due to fears that it would reinforce negative stereotypes about Muslims. The lack of religious and cultural awareness of practitioners resulted in critical needs for clients not being recognized. When participants felt misunderstood, it became a barrier to them accessing future mental health services.Not helpful at all. I felt like I was being judged. I felt like it was a waste of time. I needed an Islamic point of view. I was encouraged to consider leaving my husband. They didn’t understand me, my beliefs.
Discussion
A crucial outcome of the research was the identification of stages of help-seeking, as depicted in the Muslims’ Help-Seeking Pathways model. This model provided an overview of the general processes through which practising Muslims seek assistance, in addition to the facilitators and barriers in accessing professional treatment services. The model outlines factors that are likely to be relevant to practising Muslims’ dealing with emotional distress and indicates ways to improve their engagement with professional services. The stages identified include: recognition and identification of mental health problems, initial problem management, accessing mental health services, choosing a mental health practitioner, and experiencing mental health services. These stages are relatively consistent with previous studies of Muslims’ help-seeking processes (such as Aloud & Rathur, 2009; Khan, 2006; Youseff & Deane, 2006). Even so, some additional areas for consideration were identified that are distinct from those reported by previous research. These include the participants’ concerns regarding practitioners’ knowledge of Muslims and Islam and their attitudes toward Muslims, the advantages and disadvantages of accessing treatment with a Muslim mental health practitioner, and the impact of participants’ experiences accessing mental health services.
Informal Sources of Support
It was found that initial responses to mental health difficulties tended to include seeking informal support from family and religious leaders. This is consistent with previous studies (for example, Abu-Ras et al., 2008; Al-Darmaki, 2003; Aloud & Rathur, 2009; Al-Krenawi et al., 2000). Considering the emphasis on family relationships in Islam, it is not surprising that the participants highlighted the role of family in managing personal problems and mental health issues. While consistent with religious and cultural values, at times this could be problematic. Practitioners must be able to understand the social context of the individual and how it can be supportive, while being mindful to sensitively navigate problems that can arise due to family involvement.
Religious leaders were considered prominent sources of assistance for mental health concerns. They were seen to provide religiously and culturally congruent support and assistance. Religious leaders were also a source of spiritual healing for practising Muslims with mental health difficulties. Nonetheless, the perceived lack of formal mental health training among religious leaders was cited as a key concern by the Australian participants, as it limited their ability to provide appropriate advice and referral information. Other researchers (for example, Abu-Ras et al., 2008; Osman et al., 2005) have similarly reported a lack of mental health training among religious leaders in Western countries. Given their status and access to the community, religious leaders are ideally placed to communicate accurate and helpful information to Muslims regarding mental illness and effective treatment pathways. Therefore, the training of Muslim leaders in mental health should be a priority to better equip them to assist their communities.
The central role of the family and religious leaders illustrates the need for practitioners to consider the social and religious context of the individual. They also need to understand that religious guidance and spiritual healing can be an integral part of problem management for practising Muslim clients. The development of help-seeking models specific to Muslims, such as that presented in this research, provide a way to understand their unique help-seeking processes and more effectively identify their religious and cultural influences.
Religious Perspectives on Mental Illness as a Barrier
Despite the overall positive influence of religion upon mental health, participants were able to recognize certain interpretations of religious teachings that could be detrimental. They observed that the view that mental illness is due to supernatural causes can lead to a reluctance to access professional treatment. For example, the idea that mental illness reflects a weakness in one’s faith could be demoralizing for the sufferer. This appears to represent a form of negative religious coping (Pargament, 1997), which has been associated with distress and poorer mental and physical health outcomes (Cole, 2005; Pargament, Koenig, & Tarakeshwar, 2001; Sherman, Simonton, Latif, Spohn, & Tricot, 2005). Therefore, the role of religious perspectives for Muslims’ mental health can be complex. Perhaps such beliefs become maladaptive when they are emphasized to the extent that other possible explanations are not considered. For practitioners, this highlights a need to be mindful that certain religious beliefs may have contradictory outcomes for mental health. Practitioners who explore these religious perspectives with clients in a curious and non-judgemental manner may assist their clients to identify the potential positive and negative outcomes.
Stigma
One of the barriers identified by the participants to Muslims accessing professional treatment is the stigma associated with mental illness. Stigmatizing attitudes are common in many societies around the world and can have a detrimental impact upon individuals with a mental illness (Crisp, Gelder, Rix, Meltzer, & Rowlands, 2000). This negative impact often extends to the family and friends of the individual (Luty, Fekadu, Umoh, & Gallagher, 2006).
According to the participants, stigmatizing attitudes result in a sense of shame for individuals in acknowledging their mental health problems and accepting the need for professional treatment. This is referred to as self-stigma, where individuals internalize public attitudes (Chan & Mak, 2017). Participants considered that Muslims who are less acculturated to Australian society are more likely to be reluctant to access services due to self-stigma. Research has found a relationship between acculturation, stigma, and mental health service utilization with studies conducted in the United States, which show that ethnic minorities and immigrant families are less likely to utilize mental health services compared to Caucasian families (Mendoza, 2009), and more likely to attempt to solve problems within the family (Pham, Carlson & Kosciulek, 2010). The participants drew attention to the need for community education programs to reduce stigma towards mental illness among Muslims.
Further Research Directions
A key area that requires further investigation is the role of acculturation in the help-seeking process. Although the participants perceived that Australian Muslims with higher levels of acculturation are more willing to access mental health services, the relationship between these factors is unclear. Research in this area would need to clearly define acculturation levels to then determine the impact on help-seeking processes while taking into account other potential mediating variables, such as gender, age of migration, religiosity, education level, and prior experiences with mental illness and professional treatment services. Longitudinal research would be ideal to shed light on the impact of the acculturation process on stigmatizing attitudes. Such research needs to consider important differences between immigrant groups, such as previous mental health conditions and experiences with mental health treatment.
This research focused on the perspectives and experiences of practising Muslims. It is therefore not known whether the perspectives of non-practising Muslims would differ substantially from those of practising Muslims. Investigations that compare these two groups would be of value. Such research could inform the development of effective treatment approaches for Muslims of varying levels of religiosity.
Limitations
Despite the strengths of a mixed-model study, the research was not without limitations. The use of convenience samples, particularly for the interviews, may not have provided an accurate representation of Muslims generally. The sample size for the face-to-face interviews was relatively small. Therefore, it is difficult to make broad generalizations about such a large, heterogeneous group of people. Nonetheless, the sample compared favorably with most other qualitative studies involving Muslims (such as Weatherhead & Daiches, 2010). Also, previous studies have tended to focus on one ethnic group (for example, Aflakseir & Coleman, 2009; Ai et al., 2003; Aloud & Rathur, 2009; Padela & Heisler, 2010; Youssef & Deane, 2006), whereas this research represented varied cultural and ethnic influences. A limitation of the survey was that it was not tested for internal consistency, which may have limited its validity; however, the purpose of the survey was to assess whether attitudes and opinions present among the interview participants were also evident among a larger and diverse group of Australian Muslims.
Conclusion
Regarding help-seeking for Australian Muslims, a general knowledge of mental health problems was considered essential for individuals to recognize their symptoms and the need for help. Respondents indicated that religious coping and spiritual treatment were integral to their efforts to manage mental health problems. Religious leaders were described as playing an important role for Muslim communities in providing religious guidance to address personal difficulties. The family was identified as a primary source of advice and support, reflecting its central role for Muslims. Some participants expressed positive views regarding mental health services, yet they typically faced a range of significant barriers in accessing professional help. Furthermore, decisions to seek help from either a Muslim or a non-Muslim practitioner complicated the help-seeking process. Once mental health assistance had been accessed, these treatment experiences either challenged or reinforced the barriers. In instances where participants felt understood by the practitioner, this fostered a sense of safety and trust. On the other hand, experiences where practitioners lacked awareness of religious and cultural issues reinforced barriers to accessing services. Overall, the data revealed the powerful impact of positive contact with mental health service providers in shifting barriers to accessing professional treatment. These findings highlight areas to challenge barriers for Muslims accessing professional mental health services.
References
Abu-Raiya, H. (2013a). The psychology of Islam: Current empirically based knowledge, potential challenges, and directions for future research. In K. I. Pargament (Ed), APA handbook of psychology, religion, spirituality (Vol 1): Context, theory, and research (pp. 681–695). Washington: American Psychological Association.
ABS. (2016). Religion in Australia: 2016 census data summary. Retrieved from: http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2071.0˜2016˜Main%20Features˜Religion%20Data%20Summary˜70http://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2071.0˜2016˜Main%20Features˜Religion%20Data%20Summary˜70
Abu-Ras, W., Geheith, A., & Cournos, F. (2008). The Imam’s role in mental health promotion: A study at 22 mosques in New York City’s Muslim community. Journal of Muslim Mental Health, 3, 155–176. http://dx.doi.org/10.1080/15564900802487576http://dx.doi.org/10.1080/15564900802487576
Al-Darmaki, F. R. (2003). Attitudes towards seeking professional psychological help: What really counts for United Arab Emirates university students. Social Behavior and Personality: An International Journal, 31(5), 497–508. https://psycnet.apa.org/doi/10.2224/sbp.2003.31.5.497https://psycnet.apa.org/doi/10.2224/sbp.2003.31.5.497
Al-Krenawi, A. (2002). Mental health service utilization among the Arabs in Israel. Social Work in Health Care, 35, 577–590. https://doi.org/10.1300/j010v35n01_1https://doi.org/10.1300/j010v35n01_1
Al-Krenawi, A., & Graham, J.R. (2000). Culturally sensitive social work practice with Arab clients in mental health setting. Health and Social Work, 25, 9–22. https://doi.org/10.1093/hsw/25.1.9https://doi.org/10.1093/hsw/25.1.9
Aloud, N., & Rathur, A. (2009). Factors affecting attitudes toward seeking and using formal mental health and psychological services among Arab Muslim populations. Journal of Muslim Mental Health, 4, 79–103. https://psycnet.apa.org/doi/10.1080/15564900802487675https://psycnet.apa.org/doi/10.1080/15564900802487675
Aly, A. (2010). Fear, victimisation and identity: The community victimisation perspective and social inclusion of Australian Muslims. In A. Yasmeen (Ed.), Muslims in Australia: The dynamics of exclusion and inclusion (pp.79–95). Carlton: Melbourne University Press.
Bloemraad, I., Kortewag, A., & Yurdakul, G. (2008). Citizenship and immigration: Multiculturalism, assimilation, and challenges to the nation-state. Annual Review of Sociology, 34, 153–179. http://dx.doi.org/10.1146/annurev.soc.34.040507.134608http://dx.doi.org/10.1146/annurev.soc.34.040507.134608
Chan, K., & Mak, W. (2017). The content and process of self-stigma in people with mental illness. The American Journal of Orthopsychiatry, 87(1), 34–43. https://doi.org/10.1037/ort0000127https://doi.org/10.1037/ort0000127
Ciftci, A., Jones, N., & Corrigan, P. W. (2013). Mental health stigma in the Muslim community. Journal of Muslim Mental Health, 7, 17–32. https://doi.org/10.3998/jmmh.10381607.0007.102https://doi.org/10.3998/jmmh.10381607.0007.102
Cole, B.S. (2005). Spiritually-focused psychotherapy for people diagnosed with cancer: A pilot outcome study. Mental Health, Religion & Culture, 8, 217–226. https://doi.org/10.1080/13694670500138916https://doi.org/10.1080/13694670500138916
Crisp, A. H., Gelder, M. G., Rix, S., Meltzer, H. I., & Rowlands, O. J. (2000). Stigmatisation of people with mental illnesses. The British Journal of Psychiatry, 177, 4–7. https://doi.org/10.1192/bjp.177.1.4https://doi.org/10.1192/bjp.177.1.4
Dunn, K., Forrest, J., Burnley, I., & McDonald, A. (2004). Constructing racism in Australia. Australian Journal of Social Issues, 39(4), 409–430. https://doi.org/10.1002/j.1839-4655.2004.tb01191.xhttps://doi.org/10.1002/j.1839-4655.2004.tb01191.x
Dunn, K., Atie, R., Mapedzahama, V., Ozalp, M., & Aydogan, A.F. (2015). The resilience and ordinariness of Australian Muslims: Attitudes and experience of Muslims report. Penrich, NSW: Western Sydney University.
Farooqi, Y. N. (2006). Traditional healing practices sought by Muslim psychiatric patients in Lahore, Pakistan. International Journal of Disability, Development and Education, 53(4), 401–415. https://psycnet.apa.org/doi/10.1080/10349120601008530https://psycnet.apa.org/doi/10.1080/10349120601008530
Fischer, E. H., & Turner, J. L. (1970). Orientations to seeking professional psychological help: development and research utility of an attitude scale. Journal of Consulting and Clinical Psychology, 35(1), 79–90. https://doi.org/10.1037/h0029636https://doi.org/10.1037/h0029636
Geerlings, L. R., C., Thompson, C. L., Bouma, R., & Hawkins, R. (2017). Cultural competence in clinical psychology training: A qualitative investigation of student and academic experiences: Cultural competence in clinical psychology training. Australian Psychologist, 1, 1–10. https://doi.org/10.1111/ap.12291https://doi.org/10.1111/ap.12291
Graham, J. R., Bradshaw, C., & Trew, J.L. (2008). Social worker’s understanding of the immigrant Muslim client’s perspective. Journal of Muslim Mental Health, 3(2), 125–144. https://doi/org/10.1080/15564900802487527.https://doi/org/10.1080/15564900802487527
Groves, R. M., Fowler Jr., F. J., Couper, M. P., Lepkowski, J. M., Singer, E., & Tourangeau, R. (2009). Survey methodology (2nd ed.). New York: Wiley.
Hassan, R. (2015). Australian Muslims: A demographic, social and economic profile of Muslims in Australia. Adelaide: International Centre for Muslim and non-Muslim Understanding, University of South Australia.
Hopkins, L. (2011). A contested identity: Resisting the category Muslim-Australian. Immigrants & Minorities, 29, 110–131. https://doi.org/10.1080/02619288.2011.553139https://doi.org/10.1080/02619288.2011.553139
HREOC. (2004). Isma – listen: National consultations on eliminating prejudice against Arab and Muslim Australians. Sydney: Human Rights and Equal Opportunity Commission.
Hsieh, A. L., & Bean, R. A. (2014). Understanding familial/cultural factors in adolescent depression: A culturally-competent treatment for working with Chinese American families. The American Journal of Family Therapy, 42(5), 1–15. https://doi.org/10.1080/01926187.2014.884414https://doi.org/10.1080/01926187.2014.884414
Huey, S. J., Tilley, J. L., Jones, E. O., & Smith, C. A. (2014). The contribution of cultural competence to evidence-based care for ethnically diverse populations. Annual Review of Clinical Psychology, 10, 305–338. https://doi.org/10.1146/annurev-clinpsy-032813-153729https://doi.org/10.1146/annurev-clinpsy-032813-153729
IWWCV. (2008). Race, faith and gender: Converging discriminations against Muslim women in Victoria. The ongoing impact of September 11 2001. A summary report on racism against Muslim women. Melbourne: Islamic Women’s Welfare Council of Victoria.
Kalek, S., Mak, A. S., & Khawaja, N.G, (2010). Intergroup relations and Muslims’ mental health in Western societies: Australia as a case study. Journal of Muslim Mental Health, 5(2), 160–193. http://dx.doi.org/10.1080/15564908.2010.487722http://dx.doi.org/10.1080/15564908.2010.487722
Keshavarzi, H., & Haque, A. (2013). Outlining a psychotherapy model for enhancing Muslim mental health within an Islamic context. International Journal for the Psychology of Religion, 23(3), 230–249. https://doi.org/10.1080/10508619.2012.712000https://doi.org/10.1080/10508619.2012.712000
Khawaja, N. G. (2007). An investigation of the psychological distress of Muslim migrants in Australia. Journal of Muslim Mental Health, 2, 39–56. https://doi.org/10.1080/15564900701238526https://doi.org/10.1080/15564900701238526
Khan, Z. (2006). Attitudes toward counselling and alternative support among Muslims in Toledo, Ohio. Journal of Muslim Mental Health, 1, 21–42. https://doi.org/10.1080/15564900600654278https://doi.org/10.1080/15564900600654278
Kira, I. A., Lewandowski, L., Ashby, J. S., Templin, T., Ramaswamy, V., & Mohanesh, J. (2014). The traumatogenic dynamics of internalized stigma of mental illness among Arab America, Muslim, and refugee clients. Journal of the American Psychiatric Nurses Association, 20(4), 250–266. https://doi.org/10.1177/1078390314542873https://doi.org/10.1177/1078390314542873
Knifton, L. (2012). Collective wellbeing in public mental health. Perspectives in Public Health, 135(1), 24–26. http://dx.doi.org/10.1177/1757913914563247http://dx.doi.org/10.1177/1757913914563247
Krosnick, J. A., & Presser, S. (2010). Question and questionnaire design. In P. V. Marsden & J. D. Wright, (Eds.). Handbook of survey research (2nd ed., pp. 263–314). Bingley: Emerald.
Mallinger, J.B., & Lamberti, J. S. (2010). Psychiatrists’ attitudes toward and awareness about racial disparities in mental health care. Psychiatric Services, 61(2), 173–179. https://doi.org/10.1176/ps.2010.61.2.173https://doi.org/10.1176/ps.2010.61.2.173
Mendoza, F. S. (2009). Health disparities and children in immigrant families: A research agenda.” Pediatrics, 124(3), 187–195. https://doi.org/10.1192/bjp.177.1.4https://doi.org/10.1192/bjp.177.1.4
Morgan, V., & Poynting, S. (2012). Introduction: The transnational folk devil. In G. Morgan, S. Poynting & R. Holten (Eds.), Global Islamophobia: Muslims and moral panic in the West (pp. 1–14). Surrey, England: Ashgate.
Osman, M.A., Milstein, G., & Marzuk, P.M. (2005). The Imam’s role in meeting the counseling needs of Muslim communities in the United States. Psychiatric Services, 56(2), 202–205. http://dx.doi.org/10.1176/appi.ps.56.2.202http://dx.doi.org/10.1176/appi.ps.56.2.202
Pargament, K. I. (1997). The psychology of religion and coping: Theory, research, practice. New York: Guilford Press.
Pargament, K. I., Koenig, H. G., & Tarakeshwar, N. (2001). Religious struggle as a predictor of mortality among medically ill elderly patients. A 2-year longitudinal study. Archive for Internal Medicine, 161, 1881–1885. https://doi.org/10.1001/archinte.161.15.1881https://doi.org/10.1001/archinte.161.15.1881
Pham, A. V., Carlson, J. S., & Kosciulek, J. F. (2010). Ethnic differences in parental beliefs of attention-deficit/hyperactivity disorder and treatment. Journal of Attention Disorders, 13(6), 584–91. https://doi.org/10.1177/1087054709332391https://doi.org/10.1177/1087054709332391
Poynting, S., & Mason, V. (2006). Tolerance, freedom, justice and peace? Britain, Australia and anti-Muslim Racism since 11 September 2001. Journal of Intercultural Studies, 27(4), 365–391. https://doi.org/10.1080/07256860600934973https://doi.org/10.1080/07256860600934973
Poynting, S., & Mason, V. (2007). The resistible rise of Islamophobia. Journal of Sociology, 43 (1), 61–86. https://doi.org/10.1177%2F1440783307073935https://doi.org/10.1177%2F1440783307073935
Punch, K. (2003). Survey research, the basics: Essential resources for social research. Thousand Oaks, CA: Sage Publications.
Ribeiro, M. D., & Saleem, S. (2010). Providing outreach services to Muslim college women. Journal of Muslim Mental Health, 5, 233–244. https://psycnet.apa.org/doi/10.1080/15564908.2010.487739https://psycnet.apa.org/doi/10.1080/15564908.2010.487739
Sherman, A. C., Simonton, S., Latif, U., Spohn, R., & Tricot, G. (2005). Religious struggle and religious comfort in response to illness: Health outcomes among stem cell transplant patients. Journal of Behavioral Medicine, 28, 359–367. https://doi.org/10.1007/s10865-005-9006-7https://doi.org/10.1007/s10865-005-9006-7
Tanhan, A. & Francisco, V.T. (2019). Muslims and mental health concerns: A social ecological model perspective. Journal of Community Psychology, 47(4), 964–978. https://doi.org/10.1002/jcop.22166https://doi.org/10.1002/jcop.22166
Thyer, B.A. (2010). Theoretical research. In: B. A. Thyer (Ed.). Handbook of social work research methods (2nd Ed, pp. 468–492). Thousand Oaks, CA: Sage Publications.
Weatherhead, S., & Daiches, A. (2010). Muslim views on mental health and psychotherapy. Psychology and Psychotherapy, 83(1), 75–89. https://doi.org/10.1348/147608309x467807https://doi.org/10.1348/147608309x467807
WHO. (2012). Risks to mental health: An overview of vulnerabilities and risk factors. Geneva, Switzerland: World Health Organization.
Yasmeen, S. (2016). The dynamics of inclusion/exclusion: Australia as a case study. In Yasmeen, S. & Markovic, N (Eds.), Muslim Citizens in the West: Spaces and Agents of Inclusion (pp. 15–32). London: Routledge.
Youssef, J., & Deane, F. (2006). Factors influencing mental-health help-seeking in Arabic-speaking communities in Sydney, Australia. Mental Health, Religion & Culture, 9(1), 43–66. https://doi.org/10.1080/13674670512331335686https://doi.org/10.1080/13674670512331335686