Introduction
Culturally appropriate mental health approaches are promoted by policy bodies nationally and internationally (National Institute for Health and Care Excellence [NICE], 2011; 2016; World Health Organization, 2013). National Health Service (NHS) frameworks have long highlighted the mental health needs of United Kingdom (UK) minority ethnic groups as a priority in the provision of culturally appropriate mental health services (Department of Health, 2005). The NICE (2016) guidelines (pg. 5) promote “community engagement approaches to reduce health inequalities, ensure health and wellbeing initiatives are effective and help local authorities and health bodies meet their statutory obligations.”
Research focused on minority ethnic young people suggests access to mental health services and service provision can be improved by involving young people in the development of services, having bilingual staff, and offering culturally appropriate psychological services (Street, Stapelkamp, Taylor, Malek, & Kurtz, 2005). Similarly, the Royal College of Psychiatrists (2017) recommends involving young people in service development to improve models of mental health care for their population. Despite calls for service providers and commissioners to work with young people and children to develop culturally appropriate services that they will use (Lavis, 2014), there remains little involvement of young people in the planning of services (Street et al., 2005).
There is a lack of data on the mental health needs of minority ethnic children and young people (Lavis, 2014). Children and young people from Black, Asian and other minority ethnic backgrounds are underrepresented in NHS Child and Adolescent Mental Health Services (e.g., Waheed & Beck, 2020). Evidence suggests that UK minority ethnic and religious groups report greater dissatisfaction with mental health services, and are more likely to disengage from mainstream mental health services, which may contribute to deterioration in their mental health (Arday, 2018; Naz, Gregory, & Bahu, 2019). Minority ethnic young people report encountering various barriers to accessing mental health services, including stigma attached to accessing mental health care (Gonçalves & Moleiro, 2012; Street et al., 2005), lack of culturally appropriate therapy services, language needs, cultural naivete among mental health professionals (e.g. lack of understanding of different cultural, ethnic, and religious needs), mistrust of services, and a general lack of understanding about mental health and what mental health services can offer (Street et al., 2005).
Mental health charities Mind and Rethink Mental Illness (2012) conducted an online survey with 1000 young people and found that 90% reported experiencing negative treatment from others because of their mental health problems; 43% reported fear of stigma had prevented them from seeking help (i.e., going to a primary care doctor (GP) or a counselor). Mistrust of statutory services and fear may also explain the low uptake of mental health services among minority ethnic young people (Lavis, 2014). Similarly, a service evaluation conducted with bereaved Middle Eastern and North African (MENA) Muslim women affected by the Grenfell Tower fire identified the following barriers to accessing mental health services following the tragedy: mistrust of all statutory services, lack of culturally appropriate therapeutic support, language barriers, formal delivery of therapy, hierarchical relationships between health care provider and client, and stigma and shame associated with mental health and accessing therapy (Hammad, El-Guenuni, Bouzir, & El-Guenuni, 2020).
There is a lack of research on culturally appropriate and coproduced therapeutic approaches for communities impacted by collective trauma and loss. The Inter-Agency Standing Committee (IASC, 2007) Guidelines on Mental Health and Psychosocial Support in Emergency Settings, developed by the United Nations (UN) and over 200 non-UN humanitarian organizations, suggests that in emergency and disaster settings assisted mourning and communal healing ceremonies are a useful response to support the affected community. Pedersen, Kienzler, and Guzder’s (2015) systematic review found that the activation and mobilization of local social support networks, such as symbolic restoration of collective processes for bereavement and grieving, alongside psychosocial support resulted in improved mental health for populations impacted by collective trauma and loss. Memorialization can provide opportunities to create space for memories relating to collective trauma and loss (Yoshida et al., 2016). Ceremonies like remembrance days, community gatherings, and customary rituals may help to restore natural community resilience (Somasundaram & Sivayokan, 2013).
In Nepal, a project called “Holding Hands” was offered to families whose loved ones had disappeared during the civil war (Robins, 2014). The project involved commemorating missing loved ones and group members choosing a meaningful memorial activity. It focused on creating a space to challenge the stigma, reduce social isolation, and encourage discussions on the emotional impact of their loved ones’ disappearances. Memorialization was found to be therapeutic, in that it can help boost psychological and emotional resilience and wellbeing (Robins, 2014). The public nature of tributes and memorialization serves the community and incorporates a social aspect. Memorialization can emphasize the value of their loved one’s memory, while helping to create distance and the continuation of their everyday lives (Robins, 2014). Other studies have similarly found that there are benefits of memorialization in settings where collective trauma and loss have occurred. Following an earthquake in Japan, children who attended memorial services were found to have significantly higher post-traumatic growth compared to children who had not attended (Yoshida et al., 2016).
Recent NICE Guidelines indicate that there is insufficient evidence for art-based therapy for post-traumatic stress disorder, although the evidence base is growing for creative art-based therapies, and it can be a useful way to engage young people who are reluctant to engage in traditional trauma therapies. Approaches utilizing creative arts have been found to aid recovery for young people affected by collective trauma and loss (e.g., Barath, 1996; Mohr, 2014; Ugurlu, Akca, & Acarturk, 2016). The use of creative arts therapy was found to be effective in reducing traumatic stress, depression, and trait anxiety symptoms among displaced war-affected Syrian refugee children (Ugurlu et al., 2016). Following an earthquake in Peru, creative arts approaches were found to help young people make meaning of their traumatic experiences; it improved their mood, and helped to affirm that they had survived (Mohr, 2014).
Grenfell Tower Fire: Community Context and Background
The Grenfell Tower fire occurred in June of 2017 in North Kensington, a neighborhood in the Royal Borough of Kensington and Chelsea (RBKC) of London. The Grenfell Tower fire was one of the worst fires to affect the UK in decades; 72 people died (Shildrick, 2018), with reverberating mass trauma, loss, and large-scale displacement of survivors.
RBKC is the richest borough in the UK, and is often referred to as a “tale of two cities” due to major economic inequalities that prevail in the borough, where there are extreme levels of poverty and wealth (Cornish, 2021; Shildrick, 2018). Several hundreds of thousands of pounds sterling were cut from Grenfell Tower’s refurbishment budget resulting in cheaper flammable external cladding being installed (Cornish, 2021; Guardian, 2019). At the time of writing (2021), the Public Inquiry (an official government investigation that deals with matters of public concern) into the Grenfell Tower fire is ongoing. The Public Inquiry confirmed that this flammable cladding was why the fire spread so rapidly (Cornish, 2021; Grenfell United, 2021) and why the smoke that filled the single staircase exit was so deadly and impenetrable (Cornish, 2021).
INQUEST, a national charity focused on state-related deaths (Cornish, 2021), and Grenfell United (2021) highlighted how recommendations from the inquest of a similar cladding fire at Lakanal House in 2009 were not implemented; had such recommendations been followed, it could have prevented the Grenfell Tower fire. Residents had previously and often raised concerns about the fire safety of Grenfell Tower with their landlord but no action was taken (Cornish, 2021; Grenfell United, 2021).
Grenfell United is a group of survivors and bereaved families from the Grenfell Tower fire (Grenfell United, 2021b). Grenfell United represents bereaved families and survivors and campaign for justice, change, and safe homes (Grenfell United, n.d.). Their areas of focus are policy and government legislation regarding fire safety and inequalities in social housing (Cornish, 2021). They focus on issues of collective importance which includes the removal of flammable cladding from existing buildings and banning the use of such in new construction, identifying the cause of the Grenfell fire, and that fire safety recommendations are better implemented nationally (Cornish, 2021). They also emphasize improving mental health provision for the impacted community.
Grenfell United reported a “cycle of inaction and indifference” (Guardian, 2021, para. 12) and that the government has been unresponsive to the bereaved and survivors’ fire safety recommendations (Cornish, 2021; Grenfell United, 2021; Guardian, 2019). Survivors and the bereaved have also called for an examination of the impact of race, class, and poverty on the Grenfell tragedy (British Broadcasting Corporation [BBC], 2020). Leslie Thomas, a lawyer who represents bereaved families, stated that the “Grenfell fire did not happen in a vacuum … A majority of the Grenfell residents who died were people of colour … Grenfell is inextricably linked with race … [in addition] the community affected was predominantly working-class.” (BBC, 2020, para. 5–7, para. 9). The statistics gathered by the police investigation and Grenfell United indicate that 70% of the people that died in the fire were Muslim (Grenfell United, personal communication, September 19, 2018); 85% of people who died in the fire were from Black and minority ethnic backgrounds (Guardian, 2020). Many have drawn attention to how the Grenfell Tower, a single neglected council block, is symbolic of the UK’s wider structural and systemic problems concerning the national housing crisis, austerity, and social inequalities (Cornish, 2021; Guardian, 2019).
Cornish (2021) has highlighted the difficulty in finding the appropriate terminology to describe the Grenfell Tower fire, noting the various terms used ranging from ‘disaster’ to ‘crime’ and ‘catastrophe’.
Project Facilitators’ Backgrounds
The group was co-developed and co-facilitated by the first three authors. The first author is a key community member and a Darija-speaking family systemic practitioner at NHS GHWS children and young people’s team. The second author is a key community member and a Darija-speaking young people’s counsellor at MCWG. The third author is a youth worker experienced in working in psychologically informed ways at Family Action’s Grenfell Well Community Service. Three of the authors, two of whom were also group facilitators, are directly impacted by the Grenfell Tower fire and are part of the Grenfell community. The first author (group facilitator) and the fourth author’s family survived the fire after nearly dying; they also experienced non-familial bereavements in relation to the fire. The second author’s (group facilitator) family perished in the fire.
Service Context
North Kensington has a diverse community, with large Arabic-speaking and Moroccan Muslim groups among them. There is a high percentage of minority faith and ethnic groups living in the RBKC (RBKC, 2010a, 2010b); one in 12 of the borough’s population identify as Muslim (RBKC, 2010b). After English, Arabic is the second most common language spoken in the borough (RBKC, 2010c).
A gap in the provision of culturally appropriate support was identified for children and young people affected by the fire, following feedback from some sections of the communities, who were requesting informal culturally appropriate and faith informed therapeutic support. Studies have found that adolescents from minority ethnic backgrounds tend to prefer informal social support to meet their mental health needs (e.g., Gonçalves & Moleiro, 2012).
Together For Grenfell focuses on community consultation to inform the Grenfell response, providing culturally appropriate mental health services, and supporting collaborative and partnership work between statutory services, community organizations, and affected community members. The therapeutic group described within this paper was coproduced through the Together For Grenfell partnership, a collaboration between the NHS Grenfell Health and Wellbeing Service (GHWS) Children and Young People’s team (first author), and two community organizations: Making Communities Work and Grow (MCWG; second author), and Family Action (third author), and bereaved Moroccan Grenfell-affected young community members; many of the latter group were not engaging with or were reluctant to engage with mainstream mental health services. The fourth author developed and managed Together For Grenfell. The fifth author worked at GHWS and led service evaluations for Together For Grenfell projects.
The GHWS is part of Central North West London (CNWL) NHS Foundation Trust and was established as part of the response to the Grenfell Tower fire. It offers a range of therapies and support to people of all ages who have been affected by the tragedy. Family Action provides support to people and families experiencing poverty and social isolation and disadvantage. Family Action’s Grenfell Well Community Service offers tailored practical, emotional, and financial support to individuals and families directly affected by the Grenfell Tower fire. MCWG is a local community organization working mostly with young people from minority ethnic backgrounds in RBKC. MCWG provides recreational and learning opportunities to young people who may feel disengaged, and focuses on trying to address poverty, unemployment, and lack of educational support.
Aims of the Group and Service Evaluation
Many services and community organizations deliver innovative community psychology and/or culturally appropriate psychological services; however, these projects are not well documented in the literature. There is a lack of research on culturally appropriate and coproduced therapeutic approaches in general, especially for communities impacted by collective trauma and loss. Such research is notably lacking among populations of children and young people, Muslims, and Moroccans. This project hopes to address some of these gaps. The aims of the group and service evaluation are twofold and as follows:
To coproduce a culturally appropriate therapeutic group that is responsive to the needs of young bereaved Grenfell-affected Moroccan communities and to address the barriers reported in accessing mental health services.
To assess the impact and participant experience of a coproduced therapeutic group approach for a group of young bereaved Moroccan Grenfell-affected community members, and to evaluate whether it improved access to mental health services.
Method
Theoretical Framework and Cultural Adaptation
The therapeutic group adopted an integrative approach utilizing community psychology principles, systemic/narrative approaches, collective memorialization, Teaching Recovery Techniques (TRT stabilization; Smith, Dyregrov, & Yule, 2018), creative arts therapies, and a combination of bottom-up (Hwang, 2009) and top-down (Bernal, Bonilla, & Bellido, 1995) approaches. Coproduction was central to our approach; coproduction is when professional and user knowledge is combined to design and deliver services (Boyle & Harris, 2009). We adopted a strengths-based approach that situated their personal suffering in its socio-political context (Reynolds, 2020) and rejected a deficit-based perspective that medicalized their suffering.
Community psychology focuses on the person’s socio-political and material context, how social systems interact to impact on wellbeing, and how communities/people can influence systems and structures (Bryne, 2020). Community psychology approaches move away from individualized, biomedical, and Eurocentric ideas regarding distress (Bryne, 2020) and instead focus on prevention, work with different levels, acknowledge and build upon community resources, strengths, and social capital, and emphasize the role of the group to bring about social change (Bryne, 2020). The group was informed by community psychology principles (Kagan et al., 2019; Orford, 2008) as reflected by our efforts to try to improve access and service provision for marginalized groups, strengthen community resilience, social capital, and capacity, share resources and power, acknowledge and build upon community resources, and contextualize community experiences. Community psychology principles are also reflected by our focus on coproduction, collective approaches, supporting young people’s social action efforts, and advocating for their own and their community’s needs and contributions to shape service provision.
Narrative therapy can be considered a form of systemic therapy. Our therapeutic approach drew on Michael White’s (2005) narrative work on attending to the consequences of trauma. White’s (2005) narrative approach conceptualizes: 1) pain as testimony; 2) distress as tribute; 3) pain and distress as proclamation of response; 4) expressions of pain and distress as movement; and 5) psychological pain and distress as elements of a legacy. Psychological pain and distress are considered testimony reflecting the significance of what the individual holds precious which was violated through their experience of trauma (White, 2005). This may reflect one’s ability to maintain a relationship to all beliefs, values, purposes, hopes, dreams, aspirations, commitments, and moral visions (White, 2005). It can also be considered as part of a legacy in the context of non-responsiveness by the world around them that the trauma they and others have experienced will not be for nothing and change must occur (White, 2005). Expressions of pain and distress as movement refers to how pain can be reframed as a form of movement and resistance to oppression. It can consist of subtle forms of moving away from feeling stuck when something oppressive has happened and moving away from problem narratives stuck in time. According to White (2005), this approach supports identity development based on robustness as opposed to pathologized labels pertaining to dysfunction, and a reduction in psychological pain and distress.
Narrative therapy is about rich story development and utilizing methodologies that involve reauthoring/re-storying people’s lives (White, 1991; White & Epston, 1990). Narrative therapy considers problems to stem from a socio-political cultural history and thus clients are not considered the authors of their problems (White, 1991, 2004). This is in line with community psychology approaches. It encourages the externalization of problems and the redefining of lives and identity where the individual is not defined by their problems (White, 1989, 1991; White & Epston, 1990). The meaning which a person attributes to their experience informs their narrative or story and provides the main framework of interpretation, shaping their life and expression of aspects of their experience (White, 1991, 2004; White & Epston, 1990).
During the group we focused on externalizing conversations, finding new meaning and paths, connecting to existing knowledge and skills, and thickening subjugated stories to contradict the dominant problem-saturated narrative (Carr, 2012; White & Epston, 1990). In the findings section, we discuss in greater detail examples of how we supported the re-authoring process and thickening of subjugated narratives; some discussion on this is also woven throughout the next sections. Externalizing conversations are initiated by encouraging individuals to provide an account of the effects of the problem on their lives, including their view of themselves and their relationships (White, 1991; White & Epston, 1990). Through externalizing conversations subjugated narratives can be thickened by exploring alternative and preferred knowledges of who they might be, which is considered a unique outcome (White, 1991; White & Epston, 1990). There are numerous innovative examples of collective narrative practices for working with trauma and adversity, such as the Tree of Life, Team of Life, and narrative song writing, etc. (Dulwich Centre, n.d.).
Community Consultation and Coproduction: Identifying Barriers and Adaptations Made
The goal was to coproduce a therapeutic group with the community to address the barriers young people reported, to meet their cultural needs and support them through their experiences of trauma and loss, to promote community engagement, and improve access to mental health services and service provision.
The group was created following feedback from key community members (Grenfell-affected parents and young people) who were not engaging in mainstream mental health services. Parents individually approached the fourth author, a key community member, reporting a lack of culturally appropriate therapy for their children and that their children struggled to engage with the clinical approaches offered by their school and statutory services. The parents said their children wanted informal culturally appropriate and faith-informed emotional support. The fourth author introduced the first three authors in order to set up a group for the young people which would meet their needs. The children were invited to join the group, via a letter sent to their families. The group was referred to as a space to come together with other Grenfell-affected young people. The group development was organic and the young people defined the space and group identity. We gathered information during the check-ins on what their interests were, in order to integrate these aspects into the next session. After three months, more Grenfell-affected young people in need of support were recruited by the group members to join.
The young people reported the following barriers to accessing mental health services: mental health services being too clinical and formal, that they experienced their therapist as not understanding Islam or Moroccan culture, taking an expert position and asking too many questions, and that there was stigma attached to accessing therapy which led to them not wanting to engage with services. The young people expressed that they felt disempowered, that their voices were “invisible”, and that there was no space created for them to grieve and mourn for their loved ones who had died in the fire. Some had expressed a need to memorialize.
The group ran as a weekly informal culturally appropriate user-led therapeutic group for youth between the ages of 11 and 14 who had been affected by the Grenfell Tower fire. To address the reported barriers and needs, the group facilitators focused on memorialization, stabilization, providing a safe space to facilitate expression, witnessing of their experiences, and processing of trauma and loss. The group sessions were centered on creative and engaging activities such as icebreaker games, writing spoken word poetry or short stories, art activities, and physical movement. The group met at a community center as it was designed to be informal. The group facilitators did not take an expert position or use mental health labels to describe the project or its goals. An informal, flexible, ‘no pressure’ environment where young people could talk and listen to others was created. There was a focus on activating and strengthening social support networks through group work as recommended by the IASC (2007) guidelines and community psychology approaches (Bryne, 2020).
The group facilitators focused on providing a culturally appropriate approach. The young people expressed the importance of prayer in their grieving process and anxiety management. Most group members identified sujood (prostration), physically placing their foreheads on the ground during prayer, and connecting with God, as feeling more helpful than any therapy, therefore stabilization/grounding techniques were utilized and incorporated religious rituals.
The young people expressed the importance of Islamic beliefs and traditions in their grieving process and requested a faith-informed approach. At the group’s request, Qur’anic stories and spiritual perspectives on death were explored. The aims were to support the young people to process their loss and grief utilizing their spiritual framework. We explored their beliefs about death and the afterlife. Important Islamic concepts that the young people drew upon to thicken subjugated narratives, to reframe and make meaning out of their loss related to the following: Qadr (predestination), the purpose of trials and tribulations from an Islamic perspective, and the multiple names and qualities of Allah, in particular Al-Salaam (The Source of Peace and Safety) and Al-Adl (The Just, one that grants justice).
The young people drew on Qur’anic verses to help them make sense of the tragedy, such as “Verily with every hardship comes ease” (Qur’an 94:6) and “Allah does not burden a soul beyond that it can bear” (Qur’an 2:286). The young people also explored the Qur’anic chapter Duha which contains themes of justice, the sense of abandonment, and God’s care, compassion, and love. The use of Qur’anic verses appeared to thicken subjugated narratives about being taken care of by a higher compassionate power, as their dominant narratives emphasized feeling abandoned and unsafe with external powers (e.g., government).
The group was run in English and Darija (a language spoken in Morocco), as some of the group members preferred to express themselves in Darija. Clear and accessible language was used that included colloquial slang words spoken by the young people. In line with the IASC (2007) and Thompson and colleagues’ (2018) guidelines and community psychology principles of consulting the community on the needed response, the group was coproduced with the young people, with regular feedback from them to ensure it was meeting their needs. The young people decided the content and topics for discussion which were woven into the group sessions, thus offering a more holistic approach which covered trauma and bereavement and other aspects of psychological wellbeing such as emotional regulation and feelings of depression and anxiety. The young people were encouraged and supported to lead on some sections of the sessions when they expressed the desire to do so. It was observed that when they felt in control and involved in the session delivery, they seemed more empowered and more open to taking in the information and utilizing stabilization techniques shared in the group.
Outline of Group Phases of the Therapeutic Group
The group had three broad non-linear phases, namely engagement, memorialization, and empowerment. The three are detailed as follows:
Engagement phase
The engagement phase focused on developing trust, group bonds, establishing boundaries and co-creating a safe space and ways for the young people to express themselves. These ends were facilitated primarily through drama games, art activities, icebreakers, and group discussions. The pace was gentle due to the feedback from the young people and their previous difficulties in engaging with services. Therefore, the facilitators did not attempt to describe the events of the night of the fire until the group did so. The engagement phase took around two months due to high levels of mistrust and anger.
Memorialization phase
The young people expressed feeling extremely angry and mistrustful toward institutions and authorities. It was observed that exploring their anger helped the young people to let go of some of that emotion which then allowed a space for their overwhelming sense of loss. The young people identified memorialization as a helpful way for them to grieve. One of the aims was to create meaningful ways for the young people to be involved in the memorials and remembrance of their loved ones who had died in the fire. It was observed and reported by the young people that they were struggling to mourn, grieve, or express their emotions, their experiences of the fire, and their feelings toward the deceased. Their parents were also bereaved and traumatized by the fire, and were reported to be avoidant of talking about it when approached by their children, leaving no space to remember their loved ones. Therefore, the young people were supported to process their loss by memorializing their loved ones in ways that included writing goodbye letters to the deceased, participating in spoken word, group discussions, designing t-shirts and creating banners to use during the silent marches, and dream rescripting, which involved the young people saying goodbye to their loved ones.
The memorialization of their loved ones involved youth and ethnic culture and faith. The young people supported each other and collectively mourned together in line with Moroccan and Islamic traditions. As part of memorialization activities, the young people created an art piece with religious scriptures written and drawings of the birds of heaven; each bird contained the name of the deceased. They offered collective prayers (duaa) for the deceased. Drawing on narrative ideas, the young people were encouraged to explore the Grenfell narrative and how it impacted them individually by using poetry writing and drama therapy concepts. They created boxes which contained religious text and affirmations which were important to them, goodbye letters, poems, and grounding materials.
Approaching the first-year anniversary of the Grenfell Tower fire, the young people thought about ways in which they would like to mark the anniversary and represent their loved ones that had died. The group facilitators worked with the young people to design specific events that they could be part of. The collective efforts to work on memorialization appeared to help strengthen interpersonal bonds and provided a platform for the young people to say goodbye to their loved ones and express themselves.
As the second anniversary approached, the facilitators worked with the group to consider appropriate ways to commemorate the tragedy; this relates to the Growing Around Grief model (Tonkins, 1996) which outlines how individuals continue to experience grief as their life progresses and evolves. Therefore, the group facilitators were aware that different types of memorial events were needed for June 2019 compared to those that took place in June 2018.
Empowerment phase - graduating as ambassadors
This ongoing phase focuses on self-efficacy, hopes, empowerment, and future goals. The group concluded on the group’s one-year anniversary, with a showcase of the creative work that the young people had put together. Participants also shared with the audience the stabilization techniques they had learned during the group. The graduation ceremony event was designed to be a celebration of their achievements, their sense of empowerment, and the next step in their journey. The graduation ceremony was inspired by White’s (2005) narrative concept of definitional ceremonies and outsider witness response, which was witnessed by their families, school teachers, a Member of Parliament (MP), and the community.
During this event, they all graduated as group ambassadors. An NHS ambassador program in relation to this project was co-created with the young people, who are experts by experience. More than half of the young people chose to interview for these roles, thus giving them an authentic experience of applying for a job role; all who interviewed were successful in securing ambassadorships. The young people are reimbursed for their work in line with national guidance on service user participation. The remaining young people reported feeling ready to move on and reclaim other parts of their life that had been previously abandoned due to their difficulties post-Grenfell, such as focusing on their exams and friendships.
As part of their roles as NHS ambassadors, they have provided consultation to services, delivered workshops and talks in the community, and produced documentaries. Ambassadors have also done media interviews to raise awareness about the impact of the Grenfell tragedy, to advocate for the community’s need for justice among the general public, and to encourage people who are impacted to seek support. They have produced motivational and psychoeducational videos to raise mental health awareness and encourage young people to access support. The young people use media platforms to share their experiences of the Grenfell tragedy and the impact it had on their lives and their community, to emphasize the injustice of what happened, and to call for action. They also spoke about the need to give young people a voice and to provide informal support in non-clinical settings in a way that feels helpful for young people. They focused on re-authoring stories and building narratives of resilience within the community and advocating for young people to take ownership of their recovery and support. The NHS ambassador roles appeared to help build their confidence, sense of empowerment and work experience.
Reflections and Challenges
Having a multidisciplinary team (MDT) helped us to utilize a variety of approaches to support the young people. There were various challenges we faced facilitating this new group project. The emphasis on what therapy is expected to look like according to Eurocentric Western mainstream therapy trainings left some facilitators experiencing discomfort for not offering traditional clinical approaches and feeling under pressure to do so. We managed this by sitting with the discomfort and prioritizing the young people’s needs.
We experienced the young people as showing difficult behaviors at times, which we reframed as resistance to injustice. We were sensitive to the power dynamics and that they experienced powerlessness and experienced us as holding positions of power, therefore enactments were not interrupted to help address the power imbalance. There was a power imbalance because we were adults, professionals, held positions of power, and some of us worked in the NHS; they also experienced lots of subjugation from authorities, the community and systems around them. In addition, there were difficult dynamics between bereaved and survivors in the community which were mirrored in the group space. We created a space for them to enact this. Enactment is a systemic concept referring to situations where clinicians guide, in this case, group members to interact or talk to each other to observe and modify problematic exchanges (Minuchin, 1974). We also worked towards trying to address the power imbalance by encouraging the young people to choose the group topics, positioning the young people as the experts, and them adapting the stabilization strategies that they were expert in; we tailored resources accordingly. We managed the personal and boundary challenges by the group members by renewing and revisiting the group contract and asking the group members to decide the consequences of breaching boundaries. We also managed their lack of trust by having a longer period of engagement and focusing on building trusting relationships. In addition, we took regular breaks and the group was planned according to three phases, where we carried out reviews at intervals. Another challenge that some facilitators encountered was the difficulty in finding a neutral space – ‘a home’. We conceptualized our experiences as parallel processes reflecting some of the experiences and dynamics occurring in the wider community and what the young people were experiencing.
The young people described feeling like they had to prove their connection to the deceased. In the wider community, various labels are assigned such as “survivor” or “directly bereaved” (family bereavement), which defines what support they can access and has contributed to difficult community dynamics regarding whose grief is deemed valid; these dynamics were similarly mirrored and enacted in the group. We managed this by validating their loss, removing labels, encouraging them to bear witness to each other’s stories, and congratulating them for co-creating a space where all three sections of the Grenfell-affected community could work toward healing together, as directly bereaved, survivors of the fire, as well as bereaved members from the wider community attended this group. Two of the facilitators also represented two different parts of the community – one facilitator’s family were survivors and another facilitator had experienced a family bereavement. They modeled sharing a safe space to process the difficulties that were going on external to the group.
Having group facilitators who were directly impacted by the Grenfell fire appeared to help the young people relate to us better, as they felt we could understand what they were experiencing. It helped counteract their lack of trust in the NHS and authorities because the young people knew we were “one of them”. We demonstrated resilience beyond labels – i.e. not all impacted people are “victims”; we showed them how we utilized our pain and experiences in a way that could give back to our community. This appeared to encourage the young people to do the same via their NHS ambassadorships, where they supported other children and young people in the Grenfell community.
Although experiencing a similar trauma and loss as our clients helped build trust, connection, and empathy, it came with its own challenges. It was imperative for us to have consistent supervision and our own support to utilize a self-reflexive lens to explore group dynamics and address the complex systemic issues that arose. For example, some discussions centered on the impact of witnessing stories, how the young participants reported similar stories to our own, political discussions regarding inequalities and injustice, and the dynamics between survivors and the bereaved in the community being mirrored in our group space. Having a reflective space to work through our own triggers and dynamics, as well as working closely with the Together For Grenfell manager, helped us to deal with wider issues that occurred external to the group space.
The majority of young people also expressed that they thought that mental health professionals expected them to cry and express their distress in a particular way acceptable to society; however, they did not like crying and preferred to express their emotional pain via activism to seek justice and the arts. We also encouraged relational reflexivity by exploring how they would like people to respond when they did cry and drawing on narrative ideas regarding what emotional pain and distress may represent (White, 2005). This appeared to give permission to attendees to cry in the group, leading to more comfort with expressing vulnerability.
Participants
The group members consisted of 16 British youth of Moroccan origin between the ages of 11 and 14 who were affected by the Grenfell Tower fire. There were 1 male and 15 female participants. All reported witnessing or surviving the fire. All were bereaved in connection to the Grenfell Tower fire. The large majority (13) had lost several loved ones including family to the fire. The majority were also permanently displaced due to the fire. Two of the group members were unable to continue attending the group because they had to repeatedly move accommodation and did not participate in the focus groups.
Prior to the group, 15 group members were not engaged in any mental health services or accessing therapy; nine group members declined services and six group members had not had any contact with any mental health services. One young person was referred by her therapist to take part in the collective memorialization offered by the group.
Procedure
The group ran once-weekly sessions in the evenings between March 2018 and June 2019, with a break during summer months. A total of 43 sessions were offered. Semi-structured focus group interviews were held with 14 participants in February and June 2019 by the first three authors. Examples of focus group questions included “how did you find the group?” and “how did you find the Grenfell remembrance sessions?” The focus group interviews were transcribed. A thematic analysis (Braun & Clarke, 2006) focused on evaluating the group members’ experiences of the group. The data regarding attendance rate, referrals, and access to services/therapy before and after the group was overseen by the first author and checked on the service database; participants were also individually asked if they were accessing any services or therapy prior to group inclusion.
Prior to the service evaluation, NHS approval was obtained. All participants were verbally provided with a description of what the service evaluation involved, the purpose, and the voluntary nature of their participation. Verbal consent was gained by the participants and their parents before taking part in the service evaluation. Participants were aware that they could withdraw from the evaluation, refrain from answering any questions, that the data would be anonymized with no identifying details, and that their participation would not negatively affect their current or future access to services.
Findings
First Outcome: A Coproduced and Culturally Appropriate Therapeutic Group Improved Access to Mental Health Services and Reduced Stigma
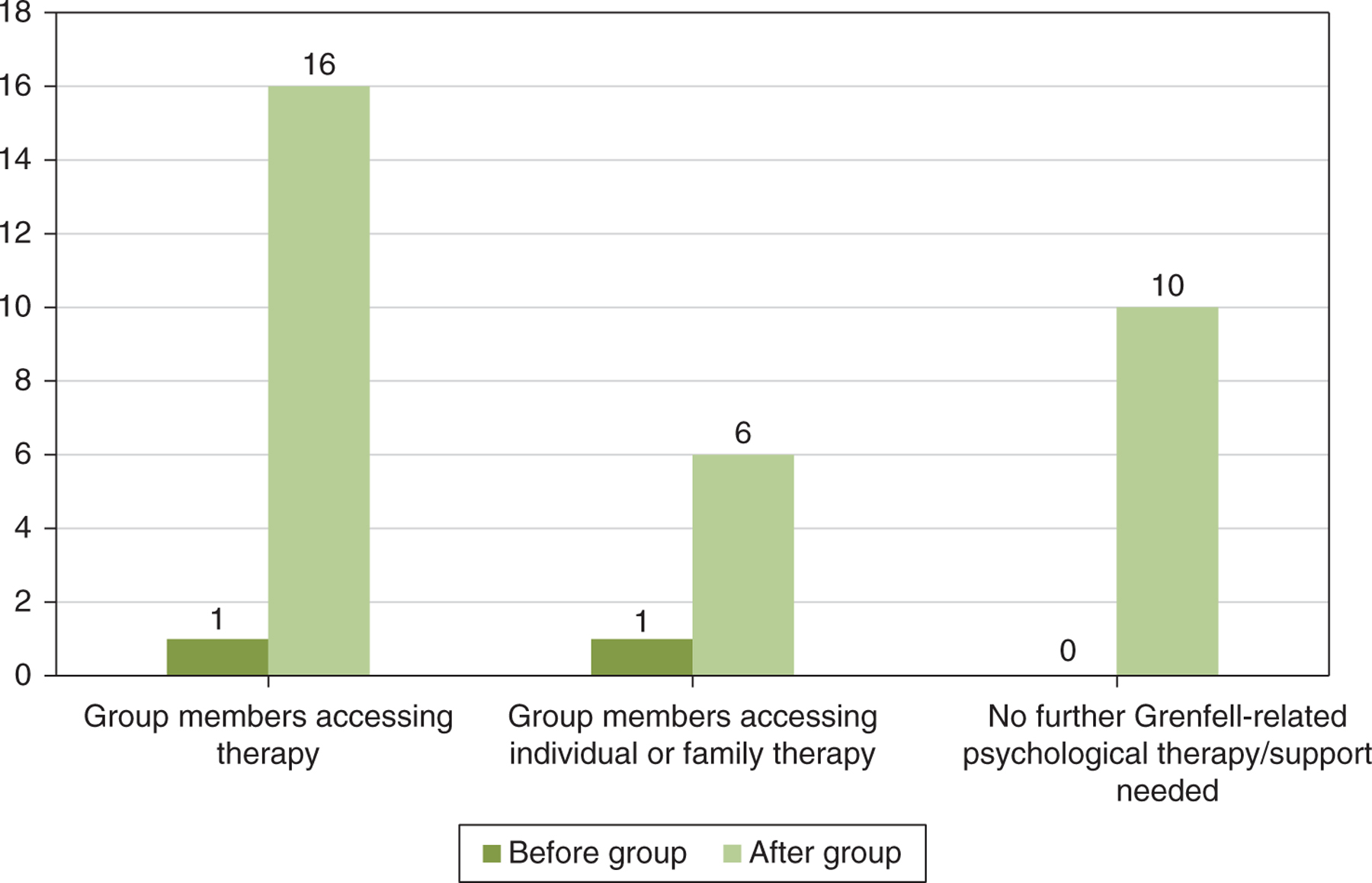
The group engaged and facilitated access to therapeutic support for 16 bereaved Moroccan young people affected by fire; the majority of whom were not previously engaging with mental health services or accessing therapy. All have since been assessed for trauma symptoms by Grenfell Health and Wellbeing Service. A 100% engagement and retention rate was attained. Over the course of a year, the average group attendance was 91%. This may suggest that a coproduced and culturally appropriate approach was received favorably by the group participants, it helped reduce the stigma associated with accessing therapeutic support, and improved access to mental health services. Having facilitators from the same community as the participants and who were also directly impacted by the fire may also explain these findings. Through their engagement in the group, six group members went on to access short-term individual or family therapy (see Figure 1). This may suggest that the group helped improve their perceptions of statutory mental health services and other forms of therapy.
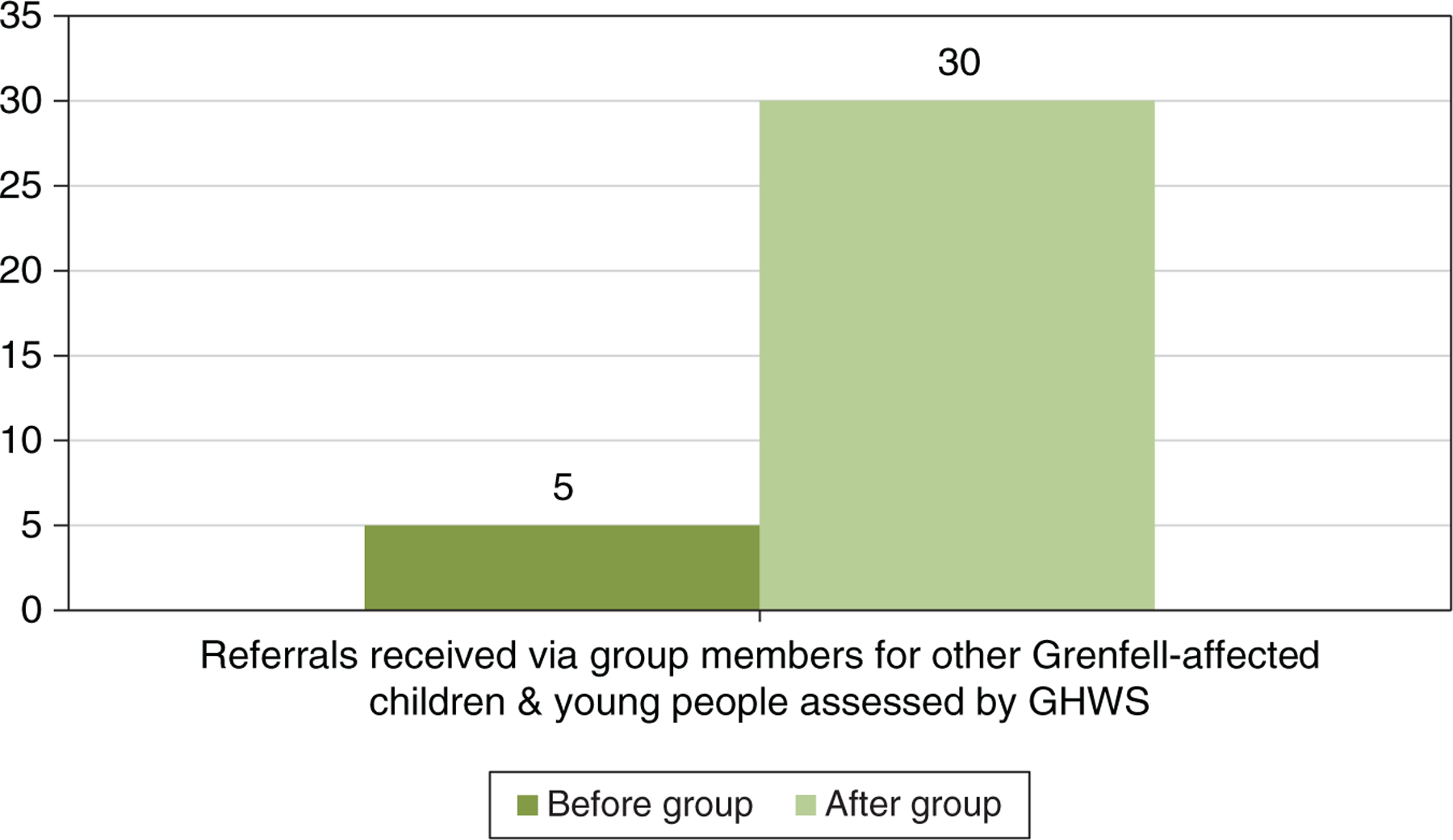
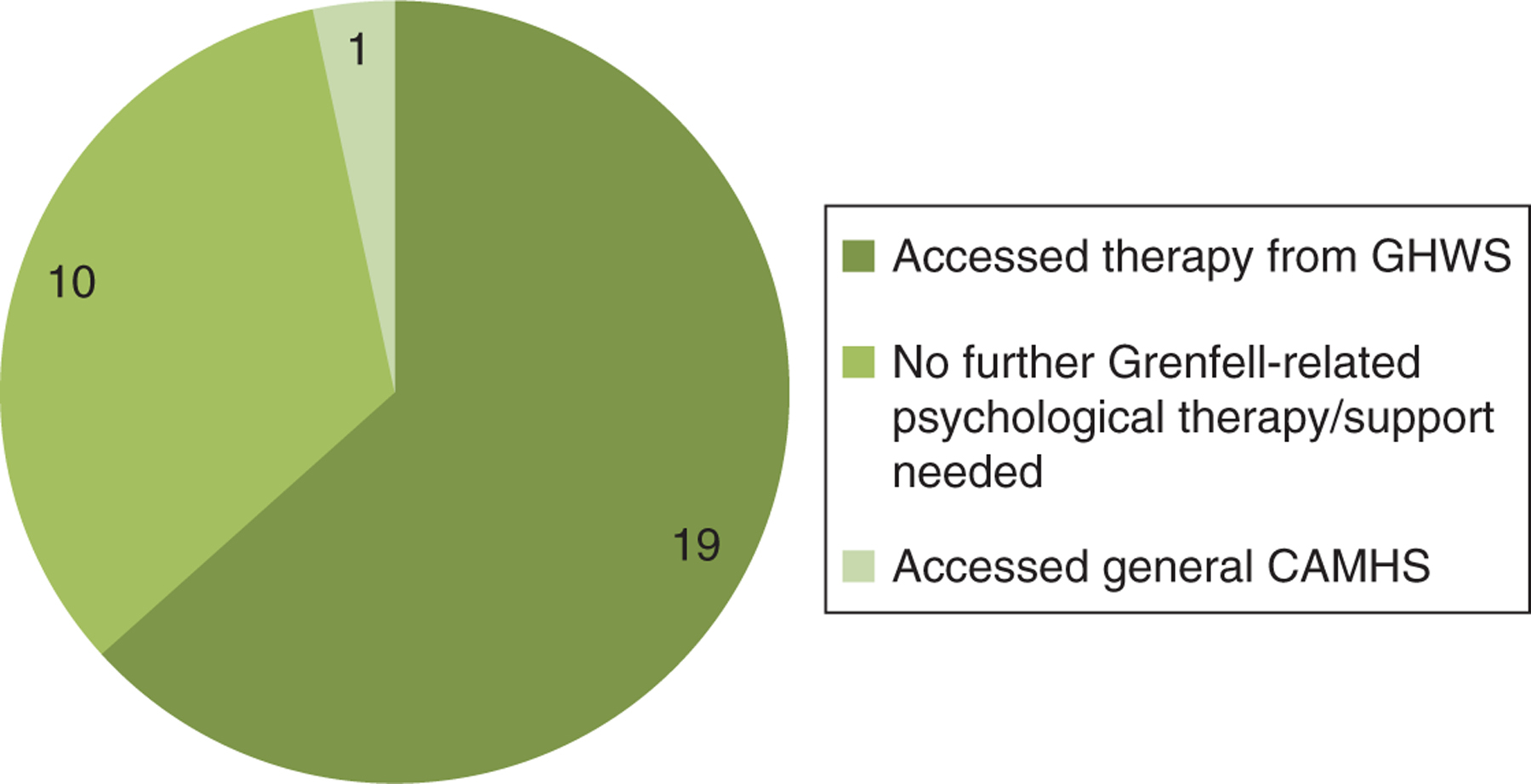
We received 30 referrals through word-of-mouth for other Moroccan Muslim children and youth between the ages of 7 and 16 affected by the Grenfell Tower fire via the group members. All have been assessed for trauma symptoms (see Figure 2) and the majority has accessed therapy through Grenfell Health and Wellbeing Service (see Figure 3).
Trauma assessments were conducted by the Grenfell Health and Wellbeing Service, Children and Young People’s team via the usual referrals pathway. This took place at the hospital where the service is based, or at a community center, depending on the client’s preference. Trauma assessments involved clinicians talking with the children and young people, speaking with their parents, and the use of outcome measures to assess their overall mental health (including trauma and complicated grief ), and what type of support to offer if needed. Assessments also involved a holistic approach and taking into account their other needs, such as physical health needs and housing issues, etc. This included signposting them to other services, or liaising with their family’s keyworker and other relevant professionals to coordinate a care plan.
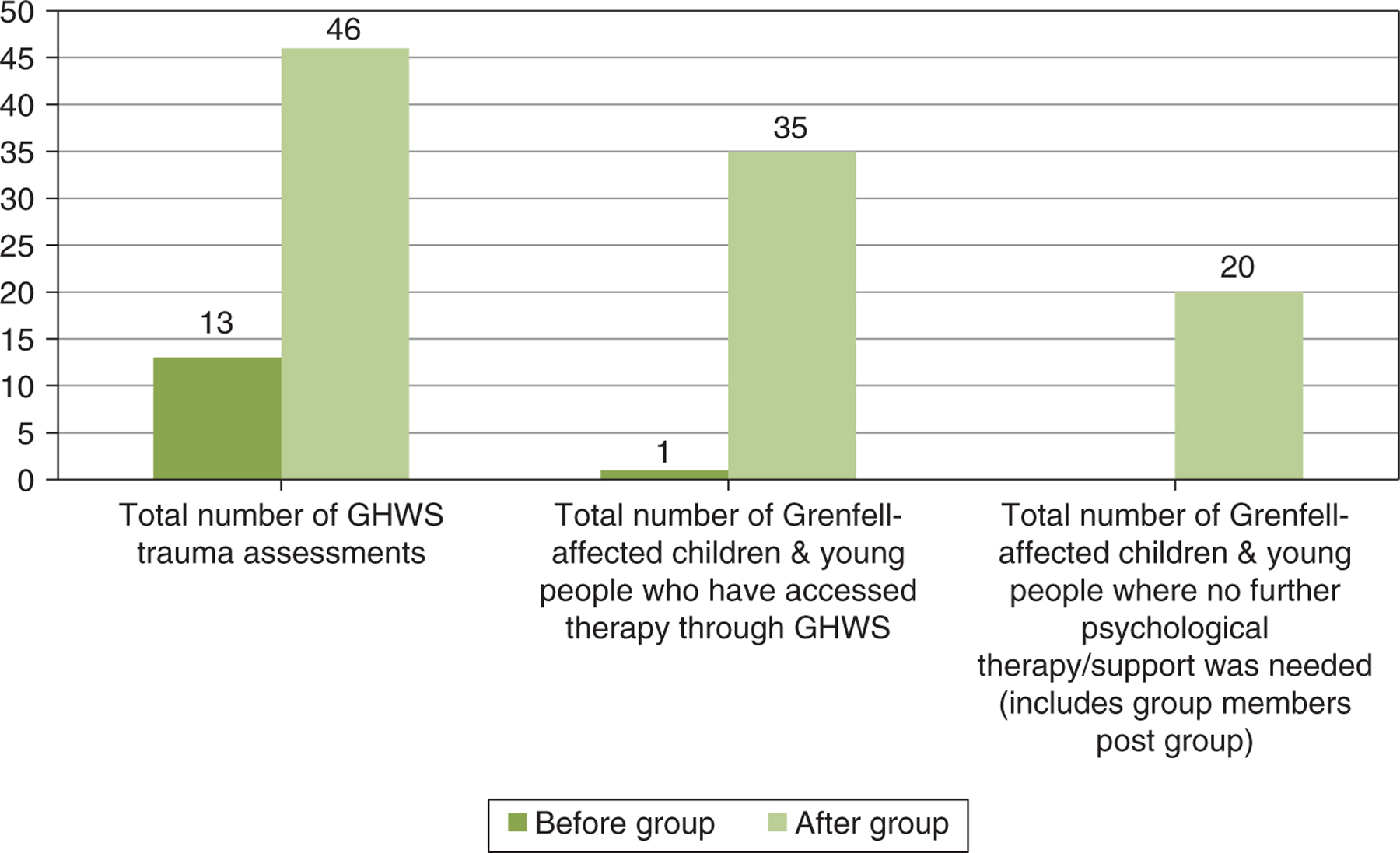
A total of 46 referrals were received for Grenfell-affected children and young people, who were not engaging with mental health/therapy services, and were assessed for trauma symptoms by Grenfell Health and Wellbeing Service (GHWS). In total, 35 children and young people have accessed therapy through GHWS via the group, and 20 children and young people required no further psychological therapy/support, which includes post group for some group members (see Figure 4).
This data suggests that a coproduced and culturally appropriate approach improved community engagement and access to mental health services for Grenfell-affected Moroccan Muslim children and young people. It helped facilitate children and young people to be assessed and to be offered support if needed and requested.
Second Outcome: Re-authoring Stories and Strengthening Subjugated Narratives
In this section we discuss the dominant narratives of the young people and how we applied narrative concepts to support the re-authoring of stories and strengthening subjugated narratives using field notes and reflections from the facilitators to explore this. We present this first to help illustrate the application of narrative practices and to provide context for the findings that follow. To avoid repetition, we do not present quotes in this section; evidence to support the theme of “re-authoring stories and strengthening subjugated narratives” can be found in outcomes three, four and five that follow.
The group members’ dominant narratives involved them feeling powerless, insignificant, unheard and “invisible”, that the world felt frightening and unsafe, and that the government wanted to get rid of them. We encouraged the noticing of subjugated narratives that focused on their resilience, compassion, power, and strength, enabling them to associate themselves with more hopeful capable empowered identities. They reported experiencing insufficient space for the performance of their new preferred stories (White & Epston, 1990), therefore we focused on facilitating spaces where they could thicken subjugated narratives.
It was important for their families, and other significant systems and people in their lives to witness their new stories in order for them to be successfully re-authored, and for the audience to contribute to new meanings and to revise and extend these new stories (White & Epston, 1990). Therefore as part of the re-authoring process we organized a graduation ceremony (White, 2005), where attendees showcased their journey to empowerment through the creative work and poetry they had created in the group, and received graduation certificates as ‘Ambassadors’. A position was also created for them to become ‘NHS Ambassadors’, where they continued these new empowered roles. As part of their NHS ambassadorships they have provided consultation to services, advocated for young people, delivered workshops and talks in the community, produced documentaries, undertaken media interviews to raise awareness about the Grenfell tragedy among the general public, and produced motivational and psychoeducational videos to raise mental health awareness and encourage youth to access support.
The young people also often referred to being described by the education system as “underachievers” and often reported the education system had expressed low expectations for them. It was therefore considered important for them to be given their graduation certificates in their re-authoring ceremony by the chief executive of their local NHS trust in the presence of their school head teacher and other significant teachers. This was important because their head teacher, teachers and loved ones witnessed their new labels and redefining of their new competent identity.
Many of the examples involved social action, activism, and advocacy by the young people, and raising awareness about the Grenfell tragedy. The young people used media platforms to share their experiences, the impact that the Grenfell tragedy had on them and their community, and the community’s need for justice. They also spoke about the need to give young people a voice and to provide informal support in non-clinical settings in a way that feels helpful for young people. Some spoke about resisting the “victim” label imposed on them.
Opportunities were facilitated for the young people to visit the House of Commons and speak directly with the Grenfell MP to share their experiences of their family’s housing problems (e.g., insecure housing, being moved from accommodation numerous times, fire safety). The young people advocated for better student mental health provision at their school by speaking directly with their head teacher about this need, holding assemblies where they shared stabilization techniques with their peers, and helped improve an initiative that allowed Grenfell-affected students to leave class if distressed so that they could have some needed space.
The group participated in Grenfell remembrance sessions, which appeared to help them process their loss and trauma. The group also participated in the monthly Grenfell remembrance silent marches as an act of collective memorialization and resisting injustice; this also connects to the narrative idea of tracing the history of refusal, whereby resistance to social injustices can help to thicken subjugated narratives (White, 1991). All of these experiences appeared to support the thickening of subjugated narratives and the re-authoring of their lives. We observed and they reported that this strengthened their confidence, resilience, and sense of power. In the next section the findings from the focus groups are discussed.
Third Outcome: Improved Emotional Expression
The findings indicated that the group helped the young people to express themselves and their emotions. Some examples of participant feedback are as follows:
I found the sessions hard, however it was very helpful and it helped me to express my emotions.
I learned how to express myself and that talking is okay.
… It makes such a difference to talk about things in here. It feels good here and it makes it easier to talk.
Fourth Outcome: The Value of Collective Memorialization and Paying Tribute to Loved Ones
The collective memorialization appeared to provide the young people with a space to express themselves and to say goodbye to their loved ones. All reported feeling empowered, listened to and able to memorialize their loved ones after they had attended the one year anniversary event as part of the group. Some participants described the value of collective memorialization as follows:
My favorite bit was writing the poems, and then me and “X” performed it. I liked how we were performing to other people so they could hear what we were saying, and I also liked that you’re writing what you’re feeling. Like, I was writing a poem and I mentioned the people who died, and it’s almost like you’re reading it to them, like they heard.
We were proud to be at the march; the world could see us and hear us.
We felt special and we were given the opportunity to be heard by taking part in the march and reading our goodbye poems.
Fifth Outcome: Recognizing Shared Grenfell-Related Experiences - Strengthening Social Support Networks and Reducing Social Isolation
Participants reported that the group created a space for them to express themselves, and it helped them to recognize shared experiences and difficulties following the Grenfell fire tragedy. They also reported how the group helped them to feel less socially isolated and to connect with others going through similar experiences, as described below:
… before I came [to the group] I sort of felt like I’m alone, but when I came and heard other people talking I felt less alone, coz I’m going through that too; I’m not the only person feeling that way.
… My mum asked me if I wanted to go to it [group] and I said I don’t wanna talk to anyone, like, I didn’t even wanna talk to my mum, and then I started to listen to others. I heard people talking about their circumstances; I started to realize like maybe it’s not just me, maybe I need to talk, like they’re opening up to me so maybe I should open up to them. So, I was like I should do the same, and it did help me coz I wanna talk to other people who understand.
My favorite part is being with people who understand pain and problems that are similar.
Sixth Outcome: Preference for Therapeutic Groups Over Individual Therapy
The group was unanimous in their preference for therapeutic support to be delivered in a group format as opposed to individual therapy. Several young people reported finding individual therapy uncomfortable and that therapeutic support in a group format helped them to feel more comfortable and at ease with expressing themselves.
I prefer this to one-to-one therapy because there are other people, coz I find it strange to just talk to one person.
I’ve got one-to-one therapy and she just stares at me, like I don’t know what to do next. I’m just there like entertainment … one-to-one [therapy] is just weird.
One-to-one therapy is awkward … in a group you can express yourself more, there’s more to say about everything.
A participant described a preference for groups because it can provide a space where people can relate to others in similar circumstances, whereas individual therapy takes place with a stranger. Sharing a space with others who were similarly impacted by the Grenfell tragedy and from the same community appeared to help improve connectedness between group members and facilitators. Two of the group facilitators are key community members and are personally affected by the Grenfell fire. Participant responses indicate that relationship allowed for greater sharing, as related below:
I did one-to-one [therapy] as well but I feel like when you do one-to-one [therapy] it’s really draining and really awkward, and I feel really weird talking to strangers about it. Coz I know you guys, you’re round the area; I know you’re personally affected by Grenfell as well, so even though we’re in a group and we can relate to others in the group, we can also relate to staff in the group as well.
Seventh Outcome: The Young People Valued the Group
The group members expressed finding the group a valuable source of support. Participants described how the group helped to reduce their stress, it enabled them to talk about issues affecting them, it provided a needed escape from life stressors, and improved their self-reflection, emotional regulation, and their journey toward healing, as described below:
I like the group; it feels like a break from everything. There’s so much stress out there, from school and everything, in here it just means we can let some of that go.
I found the sessions helpful and it made me reflect more, it made me understand what to do and what thoughts to have.
It was positive and reflective because we have come so far and also we are moving forward.
I liked the exercises because I can use what we learned at home and school to calm down.
The group also reported that they valued the cultural adaptions and faith-informed aspects to the group, which helped them to cope.
We were all of the same culture and it helped a lot with dealing with our problems.
Discussion
Our aim was to pilot an innovative way of working to improve service provision and access to mental health services for young people from diverse ethnic and faith backgrounds affected by the Grenfell Tower fire who were not accessing services. The evaluation findings indicated that the group improved community engagement and access to mental health services for a group of bereaved Moroccan-origin youth following the Grenfell fire. Participants had previously held negative views of therapy, declined or were not accessing therapy or mental health services, and reported finding services inaccessible. The evaluation findings indicate that the group appeared to help improve their ability to express themselves and their emotions, it helped them to re-author their stories and strengthen subjugated narratives, recognize their shared experiences of the Grenfell fire tragedy, strengthened their social support networks, and reduced social isolation. The young people reported valuing the group, collective memorialization, and paying tribute to their loved ones. The findings also indicated a preference for therapeutic groups over individual therapy.
The young people had a voice in shaping the delivery of the service they were receiving. The group was coproduced in collaboration with the community and the young people, and was tailored to meet the group’s cultural needs (faith and ethnic and youth culture). This may explain the findings of a consistently high group attendance, engagement and retention rates, increased uptake of therapy, referrals through word-of-mouth, and the young people reporting that they valued the group. The increased access to mental health services and the uptake of therapy suggests a reduction of stigma associated with accessing therapy and mental health services, when therapeutic approaches are culturally appropriate and coproduced with the community. It also suggests that the therapeutic group helped reauthor a new narrative about therapy and mental health services. The Royal College of Psychiatrists (2017) reports that young people value non-stigmatizing, flexible, and community-based services, which is in line with our findings.
These findings highlight how partnership work between statutory services, community organizations, and community members can help to create accessible and acceptable services for young people from diverse ethnic and faith groups (e.g., Lane & Tribe, 2010; Street et al., 2005; Thompson et al., 2018). They also align with other findings which demonstrate how culturally adapting therapies (e.g., Bhui et al., 2015; Hall, Ibaraki, Huang, Marti, & Stice, 2016; Mir, Ghani, Meer, & Hussain, 2019; Soto, Smith, Griner, Domenech Rodríguez, & Bernal, 2018) and coproduction improve access to mental health services for diverse ethnic and faith groups (e.g., Hammad et al., 2020; Nagel et al., 2009; Thompson et al., 2018). The findings also suggest that employing local people from the community who are impacted by a shared tragedy may help with community engagement and the building of trusting relationships.
Mind (2013) found that coproducing mental health services with service users was more effective for the people using them; it improved psychological wellbeing, reduced social isolation, reduced stigma regarding accessing services, and increased skills, which coincides with findings in this service evaluation. Similarly, a systematic literature review for civilian conflict-affected populations found that involving community resources and survivors in the decisions regarding support options improved mental health outcomes (Pedersen et al., 2015). Coproduction of services has also been found to utilize untapped community resources, increase capacity, provide sustainable outcomes, increase resilience, and promote the prevention of problems, as well as being able to financially compete with existing public services (Boyle & Harris, 2009). Participation and coproduction are also a core part of the children and young people’s improving access to psychological therapies project (CYP-IAPT) transformation agenda (NHS England, 2014).
Expressing emotions is considered an important part of mourning (Worden, 2010). The improved emotional expression reported by the participants may have been facilitated by the use of creative arts (Carey, 2006; Eaton et al., 2007; Pifalo, 2007; Smyth, 2015), narrative approaches (White, 2005; White & Epston, 1990), and collective memorialization. Using creative arts with trauma-affected youth can help them to access, express, process and integrate their traumatic memories (Pifalo, 2007) through kinesthetic and sensory processes (Malchiodi, 2014). Creative arts can help to create distance and contain difficult and intense emotions when tending to traumatic material, as well as supporting coping and emotional regulation techniques (Mohr, 2014; Pifalo, 2007). They can also help to provide a medium to express traumatic experiences which are difficult to verbalize or assist individuals who are not ready to directly confront their trauma (Carey 2006; Eaton, Doherty, & Widrick, 2007; Smyth, 2015). The findings regarding improved emotional expression may also be explained by the reframing of emotional distress and psychological pain as a representation of a legacy, tribute, and act of resistance to injustice (White, 2005), as well as the thickening of subjugated narratives via spaces created to express themselves (White & Epston, 1990).
When people draw on their own experiences of trauma and loss to recognize what others have been through and respond to others with compassion, it can evoke a sense of solidarity (White, 2005). This may explain the findings regarding how the group helped normalize their shared Grenfell-related experiences, reduced social isolation, and promoted social connectedness. Part of the grieving process (Worden, 2010) and understanding traumatic experiences are for these experiences to be recognized as normal responses to abnormal events. Social support networks and making connections is an important component of mourning (Worden, 2010) and recovering from trauma (Herman, 1992). Social support has also been found to be a source of resilience and has aided coping with collective trauma and loss (e.g., Hammad & Tribe, 2020a; 2020b; Somasundaram & Sivayokan, 2013). This may also explain why participants reported a preference for therapeutic groups as opposed to individual therapy; they expressed feeling more comfortable in a group setting and wished to connect with others who were also affected by the tragedy. A therapeutic group can help young people to feel safer, as they are with their peers and their peers can provide encouragement (Rambo, 2002). In the Moroccan culture, social connectedness and communal gatherings are central to the grieving process (e.g., Hammad et al., 2020; Hammad & Hamid, 2021), which may also explain these findings.
Participants reported that taking part in the one year anniversary event as part of the group helped them to feel empowered, listened to and able to memorialize and pay tribute to their loved ones. These unique outcomes suggest the thickening of subjugated narratives (White & Epston, 1990). Accepting their loss and being able to say goodbye to loved ones, in whichever way is considered appropriate for individuals is considered a key part of the grieving process (Worden, 2010). Being able to say goodbye signifies acceptance of their loss, which is particularly important as the young people never got the chance to say goodbye to their loved ones, or prepare for their deaths because of the sudden and tragic way in which they died.
Memorialization provides collective remembrance and a way to commemorate tragedies, and mourn, honor, and remember the deceased. The findings regarding the therapeutic value of collective memorialization and paying tribute to their loved ones is in line with the literature on the benefits of collective memorialization in the context of collective trauma and loss (e.g., Pedersen et al., 2015; Robins, 2014; Somasundaram & Sivayokan, 2013; Yoshida et al., 2016). Elsewhere, participation in Grenfell’s silent march has been described as “therapy” for some people (Guardian, 2018), drawing attention to the ways in which participating in calls for social action and collective remembrance of the tragedy can be therapeutic for some.
Limitations
Although the sample size is small, which may limit the generalizability of the findings, this service evaluation has contributed to several under-researched areas. We are aware that the group facilitators conducting the focus groups may have impacted on the feedback given but it was not fitting to invite external evaluators due to mistrust. We discussed the various challenges and difficulties we faced earlier on in the paper. We invited negative feedback; we are aware that the feedback was positive, which is likely to reflect our emphasis on coproduction and consultation throughout the project to ensure it was meeting their needs. Conducting pre- and post-outcome measures would have enhanced the evaluation of the impact of the group; however, it would have likely negatively affected the young people’s engagement. When conducting focus groups, there is also the risk of social desirability bias, which may have affected the feedback provided.
Implications and Future Directions
The service evaluation has highlighted the benefits of innovative, creative, and flexible ways of working to access a marginalized group and improve service provision, where the young people shaped the service delivery, which in turn improved access to mental health services for other Moroccan-origin Muslim youth. It challenges traditional Western individualistic notions of therapeutic spaces and what is considered psychological healing and therapeutic. It highlights the importance of building relationships and wrapping mental healthcare around youth-led activities (Zlotowitz et al., 2016). Coproduction draws on community resources which can create change at a community level; this was reflected by the young people’s advocacy, promoting mental health awareness, improving access to and mental health service provision for other children and young people, NHS ambassadorships, and raising awareness in public spaces about the Grenfell tragedy and the impact it has had on their community and the community’s need for justice.
Collaborative partnerships between statutory services and the community, and coproduction of psychological services with potential/service users are needed to help address health inequalities and ensure all communities can access culturally appropriate support that meets their needs. Further research on coproduced and culturally appropriate psychological projects and the tailoring of mental health services to the community needs is encouraged.
Acknowledgements:
Special thanks to the young people for taking part in the service evaluation, and to Grenfell United for their support in facilitating platforms for the young people to share their experiences. We would like to thank Robyn Doran and the senior management team at the Grenfell Health and Wellbeing Service for their support with this project, and Dr Sara Northey for her helpful feedback on the earlier draft of our manuscript. We would like to acknowledge Imane Bouzir and Dr Sara Alsaraf for their support during the initial phase of the group’s establishment.
Notes
Note: Any views expressed in this service evaluation are of the authors and do not necessarily reflect the views of their employers.
Disclosure statement: We have no conflicts of interest to disclose.
Conflicts of interest: The authors have no conflicts of interest to disclose.
References
Arday, J. (2018). Understanding mental health: What are the issues for black and ethnic minority students at university? Social Science, 7(10), 1–25. doi: 10.3390/socsci710019610.3390/socsci7100196
Barath, A. (1996). Creative therapies for war-traumatized children: 1991–95 Croatian experience. Croatian Medical Journal, 37(3), 174–184.
British Broadcasting Corporation. (2020, July 7). Grenfell Tower inquiry: Fire ‘inextricably linked with race’. Retrieved December 20, 2021, from https://www.bbc.co.uk/news/uk-53320082https://www.bbc.co.uk/news/uk-53320082
Bhui, K., Aslam, R. W., Palinski, A., McCabe, R., Johnson, M. R., Weich, S., Singh, S. P., Knapp, M., Ardino, S., & Szczepura, A. (2015). Interventions designed to improve therapeutic communications between black and minority ethnic people and professionals working in psychiatric services: A systematic review of the evidence for their effectiveness. Health Technology Assessment, 19(31), 1–173. doi: 10.3310/hta1931010.3310/hta19310
Boyle, D., & Harris, M. (2009). The challenge of co-production: How equal partnerships between professionals and the public are critical to improving public services. Retrieved on 20 December, 2021, from https://media.nesta.org.uk/documents/the_challenge_of_co-production.pdfhttps://media.nesta.org.uk/documents/the_challenge_of_co-production.pdf
Bryne, A. (2020). Ethical and professional issues in community psychology. In Tribe, R. & Morrissey, J. (Eds.), The handbook of professional, ethical and research practice for psychologists, counsellors, psychotherapists and psychiatrists (pp. 307–319). Routledge.
Carey, L. (2006). Expressive and creative arts methods for trauma survivors. Jessica Kingsley.
Carr, A. (2012). Family therapy: Concepts, process and practice (3rd Ed.). Wiley-Blackwell.
Cornish, F. (2021). ‘Grenfell changes everything?’ Activism beyond hope and despair. Critical Public Health, 31(3), 293–305. doi: 10.1080/09581596.2020.186918410.1080/09581596.2020.1869184
Department of Health. (2005). Delivering race equality in mental health care. Department of Health.
Eaton, L. G., Doherty, K. L., & Widrick, R. M. (2007). A review of research and methods used to establish art therapy as an effective treatment method for traumatized children. The Arts in Psychotherapy, 34(3), 256–262. doi: 10.1016/j.aip.2007.03.00110.1016/j.aip.2007.03.001
Gonçalves, M., & Moleiro, C. (2012). The family-school-primary care triangle and the access to mental health care among migrant and ethnic minorities. Journal of Immigrant and Minority Health, 14, 682–690. doi:10.1007/s10903-011-9527-910.1007/s10903-011-9527-9
Grenfell United. [@GrenfellUnited] (2021, October 30). Thread: 1/8 The lasting legacy of Grenfell must be meaningful structural change. Our 72 will not be remembered for what happened, but for the change our country so desperately needs. View: https://twitter.com/GrenfellUnited/status/1454426041213235206 [Tweet]. Twitter.https://twitter.com/GrenfellUnited/status/1454426041213235206
Grenfell United. (n.d.). About us. Retrieved on December 2021, from, https://grenfellunited.org.uk/about-ushttps://grenfellunited.org.uk/about-us
Guardian. (2018). Interview: Grenfell one year on: the citizen journalist and activist fighting for change. Retrieved on December 20, 2021 from https://www.theguardian.com/uk-news/2018/jun/10/the-citizen-journalist-and-silent-activist-change-grenfell-faisal-metalsi-grenfell-speaks-zeyad-credhttps://www.theguardian.com/uk-news/2018/jun/10/the-citizen-journalist-and-silent-activist-change-grenfell-faisal-metalsi-grenfell-speaks-zeyad-cred
Guardian. (2019, June 11). How Grenfell survivors came together - and how Britain failed them. Retrieved on December 20, 2021, from https://www.theguardian.com/uk-news/2019/jun/11/how-grenfell-survivors-came-together-to-change-britainhttps://www.theguardian.com/uk-news/2019/jun/11/how-grenfell-survivors-came-together-to-change-britain
Guardian. (2020, July 26). Grenfell families want inquiry to look at role of ‘race and class’ in tragedy. Retrieved on December 20, 2021, from https://www.theguardian.com/uk-news/2020/jul/26/grenfell-families-want-inquiry-to-look-at-role-of-race-and-class-in-tragedyhttps://www.theguardian.com/uk-news/2020/jul/26/grenfell-families-want-inquiry-to-look-at-role-of-race-and-class-in-tragedy
Guardian. (2021, June 14). Grenfell survivors accuse government of fire safety ‘Russian roulette’. Retrieved on December 20, 2021, from https://www.theguardian.com/uk-news/2021/jun/14/grenfell-survivors-accuse-government-of-fire-safety-russian-roulettehttps://www.theguardian.com/uk-news/2021/jun/14/grenfell-survivors-accuse-government-of-fire-safety-russian-roulette
Herman, J, (1992). Trauma and recovery. Basic Books.
Hall, G. C. N., Ibaraki, A. Y., Huang, E. R., Marti, C. N., & Stice, E. (2016). A meta-analysis of cultural adaptations of psychological interventions. Behavior Therapy, 47(6), 993–1014. doi:10.1016/j.beth.2016.09.00510.1016/j.beth.2016.09.005
Hammad, J., El-Guenuni, A., Bouzir, I., & El-Guenuni, F. (2020). The Hand of Hope: A coproduced culturally appropriate therapeutic intervention for Muslim communities affected by the Grenfell Tower fire. Journal of Muslim Mental Health, 14(2). doi:10.3998/jmmh.10381607.0014.20210.3998/jmmh.10381607.0014.202
Hammad, J. & Hamid, A. (2021). Migration and mental health of Arab communities. In Moussaoui, D., Bhugra, D., Tribe, R., & Ventriglio, A. (Eds.) Mental health and illness worldwide. Mental health, mental illness and migration. Springer.
Hammad, J., & Tribe, R. (2020a). Adaptive coping during protracted political conflict, war and military blockade in Gaza. International Review of Psychiatry, 33(1–2), 56–63. doi:10.1080/09540261.2020.174125710.1080/09540261.2020.1741257
Hammad, J., & Tribe, R. (2020b). Culturally informed resilience in conflict settings: A literature review of sumud in the occupied Palestinian territories. International Review of Psychiatry, 33(1–2), 132–139. doi:10.1080/09540261.2020.174125910.1080/09540261.2020.1741259
Inter-Agency Standing Committee. (2007). IASC guidelines on mental health and psychosocial support in emergency settings. Inter-Agency Standing Committee.
Kagan, C., Burton, M., Duckett, P., Lawthom, R., & Siddiquee, A. (2019). Critical community psychology: Critical Action and Social Change. Routledge.
Lane, P., & Tribe, R. (2010). Following NICE 2008: A practical guide for health professionals on community engagement with local black and minority ethnic (BME) community groups. Diversity in Health and Care, 7,105–114.
Lavis, P. (2014, April). The importance of promoting mental health in children and young people from black and minority ethnic communities. Retrieved from December 20, 2021, from http://raceequalityfoundation.org.uk/wp-content/uploads/2018/02/Health-Briefing-332.pdfhttp://raceequalityfoundation.org.uk/wp-content/uploads/2018/02/Health-Briefing-332.pdf
Malchiodi, C. A. (2014). Neurobiology creative interventions, and childhood trauma. In Malchiodi, C. A. (Ed.) Creative interventions with traumatized children (pp. 3–23). Guilford Press.
Mind. (2013, November 20). Co-production in mental health - why everybody wins. Retrieved from December 20, 2021, from https://www.mind.org.uk/information-support/your-stories/co-production-in-mental-health-why-everybody-wins/#.XShhiOtKjIUhttps://www.mind.org.uk/information-support/your-stories/co-production-in-mental-health-why-everybody-wins/#.XShhiOtKjIU
Mind and Rethink Mental Illness. (2012, July 12). Children and young people’s programme development: Summary of research and insights. Retrieved from December 20, 2021, from https://www.time-to-change.org.uk/sites/default/files/TTC%20CYP%20Report%20FINAL.pdfhttps://www.time-to-change.org.uk/sites/default/files/TTC%20CYP%20Report%20FINAL.pdf
Minuchin, S. (1974). Families and family therapy. Harvard University Press.
Mir, G., Ghani, R., Meer, S., & Hussain, G. (2019). Delivering a culturally adapted therapy for Muslim clients with depression. The Cognitive Behaviour Therapist, 12(26), 1–14. doi:10.1017/S1754470X1900005910.1017/S1754470X19000059
Mohr, E. (2014). Posttraumatic growth in youth survivors of a disaster: An arts-based research project. Art Therapy, 31(4), 155–162. doi:10.1080/07421656.2015.96348710.1080/07421656.2015.963487
Nagel, T., Robinson, G., Condon, J., & Trauer, T. (2009). Approach to treatment of mental illness and substance dependence in remote Indigenous communities: Results of a mixed methods study. Australian Journal of Rural Health, 17(4), 174–182. doi: 10.1111/j.1440-1584.2009.01060.x10.1111/j.1440-1584.2009.01060.x
National Health Service (NHS) England. (2014). CYP IAPT principles in CAMH services values and standards “Delivering with and delivering well”. Retrieved on December 20, 2021, from https://www.england.nhs.uk/wp-content/uploads/2014/12/delvr-with-delvrng-well.pdfhttps://www.england.nhs.uk/wp-content/uploads/2014/12/delvr-with-delvrng-well.pdf
National Institute for Health and Clinical Excellence [NICE]. (2011, May 25). Common mental health disorders: Identification and pathways to care. Retrieved on December 20, 2021, from http://www.nice.org.uk/nicemedia/live/13476/54520/54520.pdfhttp://www.nice.org.uk/nicemedia/live/13476/54520/54520.pdf
National Institute for Health and Care Excellence. (2016, March 4). Community engagement: improving health and wellbeing and reducing health inequalities. Retrieved on December 20, 2021, from https://www.nice.org.uk/guidance/ng44https://www.nice.org.uk/guidance/ng44
Naz, S., Gregory, R., & Bahu, M. (2019). Addressing issues of race, ethnicity and culture in CBT to support therapists and service managers to deliver culturally competent therapy and reduce inequalities in mental health provision for BAME service users. The Cognitive Behaviour Therapist, 12(E22). doi:10.1017/S1754470X1900006010.1017/S1754470X19000060
Orford, J. (2008). Community psychology: Challenges, controversies and emerging consensus. John Wiley & Sons.
Pedersen, D., Kienzler, H., & Guzder, J. (2015). Searching for best practices: A systematic inquiry into the nature of psychosocial interventions aimed at reducing the mental health burden in conflict and postconflict settings. SAGE Open, 5(4), 1–25. doi.org/10.1177/2158244015615164org/10.1177/2158244015615164
Pifalo, T. (2007). Jogging the cogs: Trauma-focused art therapy and cognitive behavioral therapy with sexually abused children. Art Therapy, 24(4), 170–175. doi:10.1080/07421656.2007.1012947110.1080/07421656.2007.10129471
Rambo, T. (2002). The use of creative arts in adolescent group therapy. Retrieved on December 20, 2021, from https://www.cyc-net.org/cyc-online/cycol-1002-rambo.htmlhttps://www.cyc-net.org/cyc-online/cycol-1002-rambo.html
Reynolds, V. (2020). Trauma and resistance: ‘hang time’ and other innovative responses to oppression, violence and suffering. Journal of Family Therapy, 42, 347–364.
Robins, S. (2014). Constructing meaning from disappearance: Local memorialisation of the missing in Nepal. International Journal of Conflict and Violence, 8(1), 104–118.
Royal Borough of Kensington and Chelsea. (2010a). Ethnicity. Royal Borough of Kensington and Chelsea.
Royal Borough of Kensington and Chelsea. (2010b). Faith and religion. Royal Borough of Kensington and Chelsea.
Royal Borough of Kensington and Chelsea. (2010c). Most common languages spoken. Royal Borough of Kensington and Chelsea.
Royal College of Psychiatrists. (2017, February). Good mental health services for young people. Retrieved on December 20, 2021, from https://www.rcpsych.ac.uk/docs/default-source/members/faculties/child-and-adolescent-psychiatry/fr-cap-gap-01-good-mh-services-for-young-peop.pdf?sfvrsn=606ce0ae_2https://www.rcpsych.ac.uk/docs/default-source/members/faculties/child-and-adolescent-psychiatry/fr-cap-gap-01-good-mh-services-for-young-peop.pdf?sfvrsn=606ce0ae_2
Shildrick, T. (2018). Lessons from Grenfell: Poverty propaganda, stigma and class power. The Sociological Review Monographs, 66(4), 783–798. doi:10.1177/003802611877742410.1177/0038026118777424
Smith, P., Dyregrov, A., & Yule, W. (2018). Teaching recovery techniques: Children and disaster: 8 to 18 year olds. Children and War Foundation.
Smyth, J. (2015). Creative, artistic and expressive therapies for PTSD. Retrieved on December 20, 2021, from http://www.artandhealing.org/wp-content/uploads/2015/07/PTSD-White_Paper_0323121.pdfhttp://www.artandhealing.org/wp-content/uploads/2015/07/PTSD-White_Paper_0323121.pdf
Somasundaram, D., & Sivayokan, S. (2013). Rebuilding community resilience in a post-war context: Developing insight and recommendations – a qualitative study in northern Sri Lanka. International Journal of Mental Health Systems, 7(3), 1–25. doi:10.1186/1752-4458-7-310.1186/1752-4458-7-3
Soto, A., Smith, T. B., Griner, D., Domenech Rodríguez, M., & Bernal, G. (2018). Cultural adaptations and therapist multicultural competence: Two meta-analytic reviews. Journal of Clinical Psychology, 74(11), 1907–1923. doi: 10.1002/jclp.2267910.1002/jclp.22679
Street, C., Stapelkamp, C., Taylor, E., Malek, M., & Kurtz, Z. (2005). Minority voices: Research into the access and acceptability of services for the mental health of young people from black and minority ethnic groups. Retrieved on December 20, 2021, from https://www.bl.uk/britishlibrary/~/media/bl/global/social-welfare/pdfs/non-secure/m/i/n/minority-voices-research-into-the-access-and-acceptability-of-services-for-the-mental-health-of-young-people-from-black-and-minority-ethnic-groups.pdfhttps://www.bl.uk/britishlibrary/~/media/bl/global/social-welfare/pdfs/non-secure/m/i/n/minority-voices-research-into-the-access-and-acceptability-of-services-for-the-mental-health-of-young-people-from-black-and-minority-ethnic-groups.pdf
Thompson, K., Tribe, R., & Zlotowitz, S. (2018). Guidance for psychologists on working in partnership with community organisations. British Psychological Society.
Tonkin, L. (1996). Growing around grief - another way of looking at grief and recovery. Bereavement Care, 15(1), 10. doi:10.1080/0268262960865737610.1080/02682629608657376
Ugurlu, N., Akca, L., & Acarturk, C. (2016). An art therapy intervention for symptoms of post-traumatic stress, depression and anxiety among Syrian refugee children. Vulnerable children and youth studies, 11(2), 89–102. doi:10.1080/17450128.2016.118128810.1080/17450128.2016.1181288
Waheed, H., & Beck, A. (2020). Improving BAME access to a Child and Adolescent Mental Health Service: A clinical audit. Clinical Psychology Forum 336, 52–56.
White, M. (1989). The externalizing of the problem and the re-authoring of lives and relationships. Dulwich Centre Newsletter.
White, M. (1991). Deconstruction and Therapy. In Epston, D., & White, M., Experience, Contradiction, Narrative and Imagination (pp. 109–151). Dulwich Centre Publications.
White, M. (2004). Working with people who are suffering the consequences of multiple trauma: A narrative perspective. The International Journal of Narrative Therapy and Community Work, 1, 44–75.
White, M. (2005). Workshop notes by Michael White. Dulwich Centre. Retrieved on December 20, 2021 from https://dulwichcentre.com.au/wp-content/uploads/2014/01/michael-white-workshop-notes.pdfhttps://dulwichcentre.com.au/wp-content/uploads/2014/01/michael-white-workshop-notes.pdf
White, M., & Epston, D. (1990). Story, knowledge and power. In White, M. & Epston, D., Narrative Means to Therapeutic Ends (pp. 1–37). W.W. Norton.
Worden, J. W. (2010). Grief counselling and grief therapy: A handbook for the mental health practitioner (4th Ed.). Routledge.
Yoshida, H., Kobayashi, N., Honda, N., Matsuoka, H., Yamaguchi, T., Homma, H. M., & Tomita, H. (2016). Post‐traumatic growth of children affected by the Great East Japan Earthquake and their attitudes to memorial services and media coverage. Psychiatry and Clinical Neurosciences, 70(5), 193–201. doi: 10.1111/pcn.1237910.1111/pcn.12379
Zlotowitz, S., Barker, C., Moloney, O., & Howard, C. (2016). Service users as the key to service change? The development of an innovative intervention for excluded young people. Child and Adolescent Mental Health, 21(2), 102–108. doi: 10.1111/camh.1213710.1111/camh.12137