Introduction
Cancer is a chronic and potentially terminal illness characterized by the growth of mutated cells in the body (American Cancer Society [ACS], 2019). The quality of life of cancer patients has been investigated through a variety of studies in the last decade, with the majority of them focusing on women with breast cancer (Naughton & Weaver, 2014). Breast cancer is one of the most common cancers in women worldwide, and the second leading cause of cancer deaths among women (Sun et al., 2017). According to the World Health Organization (WHO), breast cancer is the top cancer in women (International Agency for Research on Cancer [IARC], 2018).
Breast cancer is the most common cancer and the primary cause of cancer-related mortality among women in Muslim countries. The incidence in Muslim countries is low compared to the incidence in the US. However, breast cancer incidence is increasing in Muslim-majority countries (Noor et al., 2016). Also, it is important to note the significance of shame and the Hijab in Muslim countries, and the impact it may have on early screening. Iranian women are suffering from breast cancer a decade earlier, and 70% of the patients are diagnosed at an advanced stage (Farma et al., 2014). Breast cancer, or more specifically, Invasive Ductal Carcinoma (IDC), is reportedly the most common cancer in the country (Nafissi et al., 2018).
With rising early detection and more successful treatment, breast cancer survival rates continue to increase rapidly; as a result, many women find themselves troubled with the psychosocial effects of breast cancer, such as fear of progression or recurrence (Ziner et al., 2012). One of the most frequent distress symptoms of cancer survivors, and most commonly reported psychological problem, is Fear of Progression (FoP) (Herschbach & Dinkel, 2014; Mehnert et al., 2006). FoP is a life-long challenge for most survivors of breast cancer, the prevalence of which indicates that to identify its construct and prevalence, and to help survivors cope with this problem, there is a need for related interventions examination (Ziner et al., 2012).
FoP is defined as “fear, worry, or concern relating to the possibility that cancer will come back or progress” (Götze et al., 2019) and is considered one of the most prevalent and stable long‐term psychological consequences of cancer survival (Simard et al., 2013; Lebel et al., 2016).
Psychological treatments for FoP are becoming more widely studied. However, treatments that are both easily accessible and cost-effective are still uncommon (Sharpe et al., 2017; Simard et al., 2013; Maheu & Galica, 2018). There are a limited number of effectiveness studies on FoP: Cognitive-Behavioral Group Therapy (CBT) (Sabariego et al., 2011), CBT-based online self-help training (an Helmondt et al., 2016), Supportive-Experiential Group Therapy (Herschbach et al., 2010), and Acceptance and Commitment Therapy (ACT) (Hasannezhad Reskati et al., 2020). However, no study has explored the effectiveness of Emotionally Focused Couples Therapy (EFT) on FoP reduction in women with breast cancer. It is suggested that dysfunctional fear of progression can be effectively treated with brief group therapies (Herschbach & Dinkel, 2014).
Emotionally Focused Couples Therapy (EFCT or, more commonly, EFT), an intervention based on couples’ relational correction (Johnson, 2008) is a short-term, semi-accessible, cost-effective couple therapy that can be either applied to groups or separate couples (Johnson, 2005; Burgess Moser & Johnson, 2008; Johnson, 2004). It is understood that the experience of chronic diseases such as cancer is happening rather interpersonally and within a duo pattern of interactions with most loved ones. Dealing with the effects of cancer has been increasingly seen in marital relationships as both influencing and being influenced by that relationship (Wiebe & Johnson, 2016).
As explained, cancer is an illness that affects not only patients but also their partners. Thus, there is a need for more couple-based psychological or psychosocial interventions designed to help patients and their partners cope with the diagnosis and treatment of cancer. Although EFT-based treatments are unlikely to be beneficial for every cancer survivor, they do provide several advantages, including convenience, cost-effectiveness, and targeting a new sphere of treatment. Therefore, this study investigates the effectiveness of the Hold Me Tight (HMT) Relationship Enhancement Program on FoP in Iranian married women with breast cancer, with an Emotionally Focused Couple Therapy-based approach.
Methods
Study design
This was a quasi-experimental, pre-test–post-test design study recruiting experimental and control groups. The HMT intervention program was implemented in the summer of 2020.
Participants
The population of the study consisted of Muslim female patients diagnosed with stage II breast cancer who visited three renowned oncologists working with the Tehran Breast Disease Research Center (BDRC). The diagnosis criterion for breast cancer was relevant medical records registered in the oncologists’ clinics. Eventually, twenty-two couples (married for at least 5 years) with a history of mastectomy or chemotherapy in the female partner were selected to participate in the study. The couples were assigned into experimental and control groups (each containing eleven couples).
Procedure
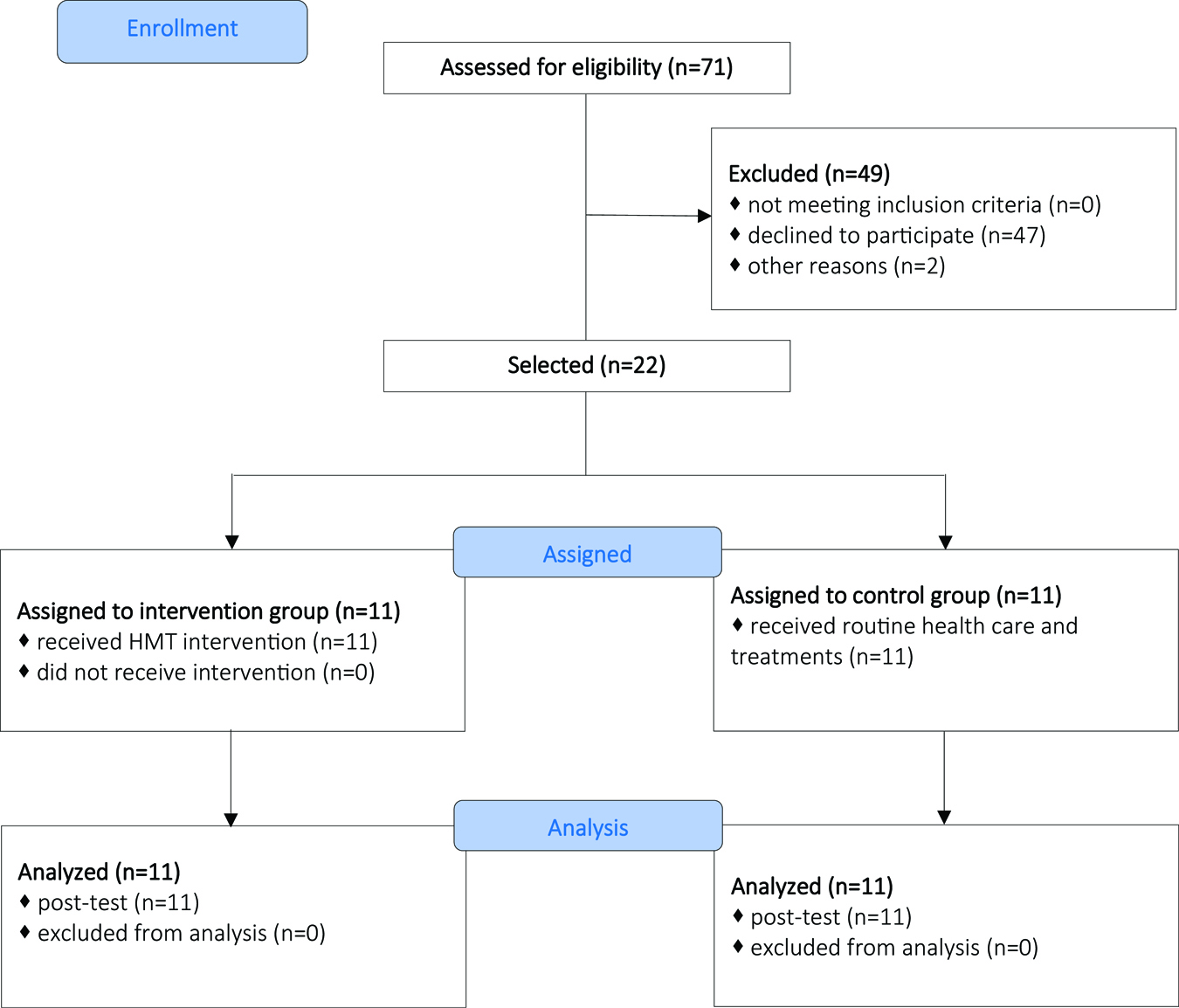
Following the approval of research in IRB of Hormozgan University of Medical Sciences, we selected a sample of Muslim couples visiting three renowned oncologists working with BDRC. In the second stage, 71 couples were assessed for their eligibility. After a brief presentation of EFT intervention and the purpose of the study, a total of 22 couples gave consent to participate in the study. In the third stage, based on the participants’ ages and psychological characteristics, the couples were assigned into experimental and control groups (each containing 11 couples). The sample size was determined using MedCalc Ver. 19.8 software based on a comparison of two means, Type I error (alpha) 0.05 and Type II error (beta, 1-power) 0.1, as well as Power 90%. Equal participants were placed in two groups (1:1 ratio). The normality was tested using the Kolmogorov-Smirnov and Shapiro-Wilk tests. Both groups were tested for normality at a confidence level of 5%, which showed the normality hypothesis of both groups was confirmed in Kolmogorov-Smirnov and Shapiro-Wilk tests. Other statistical quantities were as follows: Difference of mean score (2); Standard deviation in group 1 (1.5), and group 2 (1); Number of samples in the experimental group (n=11) and the number of samples in the control group (n=11). The mentioned software uses Cohen’s “d” for Effect Size (ES) calculation. We selected alpha 0.05 for sample size calculation. The Intra-class Correlation Coefficient (ICC) is used as a measure of the reliability of measurements. For the purpose of assessing ICC, MedCal software analyzed four rates of study subjects. The intervention group received a 6-session HMT intervention (one 120-minute session per week in two 60-minute shifts). Before and after the program, the women in both groups completed the Fear of Progression Questionnaire (FoP-Q) pre-test and post-test. The consort diagram of the study is indicated below (See Figure 1).
Ethical considerations
Informed consent and voluntary participation
Confidentiality and anonymity
Informing participants about the subject matter and method of the study
Results interpretation upon demand
Providing information and advice to participants in case of detection of mental disorder
No financial burden on the participants
Inclusion criteria:
Being married
Being Muslim
Diagnosis of stage II breast cancer for the female partner within the past 12 months
Age range of 18–55
Mastectomy or chemotherapy history
Minimum literacy
The ability to be aware and conscious enough to understand the content of the educational program
Exclusion criteria:
Any evidence of mental disorders necessitating immediate treatment
Disrupting the natural process of the intervention
Reluctance to continue with the intervention
Serious physical injury
Missing more than two sessions
Instruments
1. Fear of Progression Questionnaire (FoP-Q)
The FoP-Q is a multidimensional self-reporting questionnaire developed by Herschbach et al. (2005) using samples of patients who were suffering from breast cancer, rheumatic diseases, and diabetes mellitus. The questionnaire contains 43 items that are rated on a five-point Likert scale, ranging from never to very often. The items relate to the five dimensions: affective reactions, partnership/family issues, occupation, loss of autonomy, and coping with anxiety. The total score is calculated as the sum of the subscales’ mean scores, excluding the coping with anxiety subscale. The questionnaire (total score) has a high internal consistency (Cronbach’s α = 0.95), as well as a high test-retest reliability over one week (rtt=0.94). Lower total scores indicate more problems or impact concerning fear of progression (Herschbach & Dinkel, 2014; Kwakkenbos et al., 2012).
2. HMT Intervention Program
This evaluation study recruited an adapted version of Johnson’s (2009) couple’s group therapy treatment, the Hold Me Tight (HMT) program, which was introduced by Lynch (2015) to examine if it can help the sample of couples cope with the diagnosis and treatment process of breast cancer in a spouse or committed partner. HMT is grounded in EFT (Johnson & Greenberg, 1985a). EFT for couples (Johnson & Greenberg, 1985b) has been evaluated for couples coping with chronic illness, including cancer (McLean & Nissim, 2007; McLean et al., 2011). HMT’s brief 8-session group format (the sessions can be held over a weekend or every other week) is more cost-effective and feasible compared to a traditional EFT approach (up to 20 sessions for individual couples) for cancer patients and their partners who are often burdened with many medical appointments, cancer treatments, and their side effects. HMT is also more feasible because during a demanding cancer treatment regimen, patients are more likely to complete a shorter, structured support group intervention with their partners, rather than a longer course of couples’ therapy. HMT’s foundation in the empirically supported EFT model and its brevity suggest it is a promising intervention for couples coping with cancer. Given the unique stressors and experiences among couples coping with cancer (e.g., Li & Loke, 2014), we recruited Lynch’s (2015) reduced format (a total of six 2-hour sessions) adapted for couples coping with breast cancer in a wife or female partner. In this single-arm (HMT) evaluation study, we have addressed a gap in Iranian literature; for example, for the first time, we administered an HMT program study for couples coping with cancer.
In HMT, couples learn about their negative interactional cycles, unmet attachment needs, as well as related emotions. During group interactions and couple-based structured exercises, couples are encouraged to increase their feelings of trust and intimacy with each other. This program is an educational program to help groups of couples become more securely attached by learning more about love, attachment, and potential negative cycles of interaction and how to change them (Johnson, 2009). Lynch’s adapted version of HMT consists of six 2-hour sessions. These sessions are to be taught in conjunction with Johnson’s (2008b) book, “Hold Me Tight: Seven Conversations for a Lifetime of Love,” given to participants to read throughout the program. The session topics, such as couple’s relational conversations, include the following: (1) Recognizing the Demon Dialogues: Are We Fighting the Dragon Together?, (2) Finding the Raw Spots in the Demon Dialogues, (3) Revisiting A Rocky Moment: Becoming Open & Responsive, (4) Forgiving Injuries & Trusting Again, (5) Bonding through Sex and Touch, and (6) Caring for Yourself & Your Relationship (Lynch, 2015). An HMT therapist who bases their career on the EFT model is, in brief, a process consultant (technically called a “facilitator”). An HMT therapist facilitates the modification of a couple’s maladaptive patterns of interaction and helps them to experience underlying emotions that result from unmet attachment needs, with the primary goal of changing ‘negative cycles’ among couples and helping them attach securely and be more vulnerable (Johnson et al., 2013).
Results
The study was based on 22 couples (44 individuals) that were equally divided to the experimental and control groups, each containing 11 couples (22 individuals). As shown in Table 1, the largest number of participants (approximately 41%) were those above the age of 51. The mean age of participants in the experimental and control groups were 48.2% and 49.6% years respectively. Fifty percent of the experimental and control groups’ participants had a high school diploma; 9% had an associate degree; 30% had a B.A. or B.Sc.; and 11% had a Master’s or Ph.D. As for employment status, 64% of the participants were employed.
The demographic profile of the participants
Demographics |
Description |
Number |
Percentage |
|---|---|---|---|
Age |
20–30 |
6 |
13.63 |
31–40 |
9 |
20.45 |
|
41–50 |
11 |
25.00 |
|
51–above |
18 |
40.90 |
|
Total |
44 |
100.0 |
|
Gender |
Male |
22 |
50.00 |
Female |
22 |
50.00 |
|
Total |
44 |
100.0 |
|
Education |
High school diploma |
22 |
50.00 |
Associate degree |
4 |
9.09 |
|
B.A./B.Sc. |
13 |
29.54 |
|
Master’s & Ph.D. |
5 |
11.36 |
|
Total |
44 |
100.0 |
|
Employment status |
Employed |
28 |
63.63 |
Unemployed |
16 |
36.36 |
|
Total |
44 |
100.0 |
Table 2 shows FoP test results for both experimental and control groups in pre-test and post-test. The mean scores of the subjects in the pre-test for the experimental group (28.70 ± 88.63) and the control group (40.15 ± 93.81) were not significantly different (t(20)=-0.87, p=0.392). A comparison of the difference between post-test scores of the experimental group (35.13 ± 82.63) and the control group (41.77 ± 102.00) for FoP did not reveal a significant difference (t(20)=-0.695, p=0.495), and this indicates that the implementation of HMT program did not have a significant effect on FoP in the subjects.
The mean and standard deviation of FoP scores in pre-test and post-test of experimental and control groups
Group |
Test |
Mean |
Std. Deviation |
|---|---|---|---|
Experimental |
Pre-test |
88.63 |
28.70 |
Post-test |
82.63 |
35.13 |
|
Control |
Pre-test |
93.81 |
40.15 |
Post-test |
102.00 |
41.77 |
Due to our small sample size, normality was checked using the Shapiro-Wilk test. The distributions were normal for the experimental group (W=0.956, p-value=0.725) and the control group (W=0.944, p-value=0.569). Based on the obtained results and the visual inspection of the histogram X and Q-Q plot, it was decided to recruit a parametric test.
Before performing the analysis of covariance, we tested the homogeneity of variance assumptions and the slope of regression. Evaluations indicated that normality, homogeneity of variance, linearity, and homogeneity of regression slopes were all satisfactory. Particularly, the hypothesis of homogeneity of regression slopes was examined by independent variables and pre-test interaction, and the results showed that the variances of the two groups were equal (F=0.27, p=0.60).
Table 3 shows the mean and standard deviation of the components/dimensions of FoP variables for the control and experimental groups before and after the intervention. According to the results, none of FoP components revealed a significant change in the post-test.
Pre- and post-intervention mean and standard deviation of FoP scores for each dimension in both groups
Variable |
Period |
Intervention group (n=11) |
Control group (n=11) |
|---|---|---|---|
M ± SD |
M ± SD |
||
Affective reactions |
Pre-test |
35.18 ± 14.28 |
41.45 ± 16.09 |
Post-test |
32.27 ± 14.80 |
40.45 ± 16.84 |
|
Partnership/family issues |
Pre-test |
22.72 ± 5.86 |
21.09 ± 6.43 |
Post-test |
19.45 ± 6.43 |
20.18 ± 8.09 |
|
Occupation |
Pre-test |
14.63 ± 5.60 |
20.36 ± 10.50 |
Post-test |
14.36 ± 7.71 |
17.18 ± 9.06 |
|
Loss of autonomy |
Pre-test |
16.90 ± 6.65 |
19.09 ± 8.89 |
Post-test |
16.54 ± 8.34 |
16.00 ± 8.04 |
|
Coping with anxiety |
Pre-test |
30.45 ± 5.20 |
29.81 ± 4.60 |
Post-test |
29.63 ± 5.14 |
32.00 ± 4.47 |
As the results of Table 4 show, the difference between the pre-test–post-test scores of the experimental and control groups is not significant for the FoP variable with a value of F = 0.022 at the level of p<0.05. Therefore, HMT intervention did not affect reducing FoP in married women with breast cancer.
Results of analysis of covariance for the mean scores of pre-test and post-test for experimental and control groups in the FoP variable
Source |
Sum of Squares |
df |
Mean Square |
F |
Sig. |
Effect Size (Eta coefficient) |
Observed Power |
|---|---|---|---|---|---|---|---|
Pre-test |
21985.20 |
1 |
21985.20 |
64.39 |
0.000 |
0.77 |
1.00 |
Group |
7.36 |
1 |
7.36 |
0.022 |
0.885 |
0.001 |
0.052 |
Error |
6486.97 |
19 |
341.42 |
Discussion
This study evaluated the effectiveness of the Hold Me Tight couple’s therapy program on FoP in Iranian married women coping with breast cancer. The results of statistical analysis indicated that the mean score of FoP decreased in the experimental group compared to the control group. However, the results revealed no significant difference between the means, showing that the implementation of the HMT intervention program had no significant decreasing effect on FoP dimensions in the intervention group women as compared to the control group (p<0.05).
Mental health is the most precious asset a cancer patient/survivor possesses to cope with the disease stressors, including Fear of Progression (FoP). For married patients, emotional recognition and social support from their spouse is an invaluable source. EFT and its adapted cost-effective short-form, HMT, are considered as a promising intervention model that has targeted attachment and emotion as primary mechanisms of change in couples coping with life-threatening illnesses. Furthermore, this study was conducted on Iranian Muslims, and it can be important to consider the impact of the Hijab and shame on early screening of breast cancer. Also, such studies can highlight the importance of cultural and religious factors and even political issues to physical health.
Some studies in Iran (Javidi 2014; Javidi et al., 2012; and Javidi et al., 2014) indicated the effectiveness of EFT-based interventions on improving marital satisfaction and communication patterns in couples. Furthermore, Guarino et al. (2020) indicated that EFT models of intervention are effective in improving psychological improvement and reducing psychological manifestations of stress in women with breast cancer. Lynch’s (2015) study on the effectiveness of the EFT-based HMT program on the improvement of mental health indicators attenuated due to the cancer control process. In addition, Wiebe & Johnson (2016) reviewed the effectiveness of EFT and concluded that EFT appeared to be an effective couple therapy for couples in distress who are coping with the effects of illness in their lives, such as parents of children with chronic illnesses who reported statistically significant improvements in relationship satisfaction, communication, and intimacy after EFT (Walker, Manion, Cloutier, & Johnson, 1992). EFT researchers have examined whether EFT can be effective for couples facing cancer who are also in relationship distress. They found that EFT might be effective to improve relationship satisfaction and quality of life for couples undergoing treatment for cancer (Naaman, 2008). Mclean, Walton, Rodin, Esplen, and Jones (2013) randomized 42 couples facing terminal metastatic cancer in distressed relationships to receive EFT, as well as standard care or standard care alone. At post-treatment, couples assigned to EFT reported significantly greater improvement in relationship satisfaction, and greater improvement in the patient’s experience of their caregiver’s empathic care as compared to couples assigned to standard care alone (Mclean et al., 2013). Taken together, there is preliminary evidence that EFT can be an effective treatment for relationship distress in couples experiencing illnesses in their lives or the lives of their children.
The results of our study, in contrast with the previous studies, didn’t indicate a significant difference between the experimental and control groups. However, there might be different explanation for these results. As indicated in these studies, most of the couples were in distressing relationship, and EFT helped their relationship. It seems that the improvement in their relationships might have helped them cope with their disease. Therefore, assessing couples’ relationship satisfaction beside FoP can be helpful. There is the possibility that the sample’s relationships were not distressing. And so, we suggest assessing relationship satisfaction beside individual factors like FoP before starting intervention.
In a study on Fear of Progression, the majority of the samples (76.4%) reported low FoP (Mehnert et al., 2009). This study indicated that FoP was significantly associated with younger age, having children, disease progress, and chemotherapy. Our study sample, similar to the previous study, had low FoP (Me=88.63); and after intervention, their FoP score reduced (Mc=88.63). However, as explained in the Results section, it was not significant. The sample were relatively young (Me=43.72, Mc=48.27), were in stage II, and had finished their chemotherapy. The sample’s low FoP could be due to the reassurance that was given to the patients in the medical center. Also, they completed their medical therapy before EFT intervention. Therefore, we suggest that addressing FoP in higher stages and simultaneously with physical therapy, such as chemotherapy, might be more useful.
Furthermore, the experimental group intervention was conducted during the COVID-19 outbreak. This unpredictable condition prohibited the face-to-face presentation, and on-line sessions might have reduced the effectiveness of the HMT program. Also, the anxiety of this outbreak may have affected mechanisms through which the HMT program is supposed to reduce emotional disturbance, and affect FoP through emotional regulation.
References
American Cancer Society. (2019). Cancer facts & figures 2019. Atlanta: American Cancer Society. Retrieved on February 9, 2020, from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdfhttps://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf
Berking, M., Orth, U., Wupperman, P., Meier, L. L., & Caspar, F. (2008). Prospective effects of emotion-regulation skills on emotional adjustment. Journal of Counseling Psychology, 55(4), 485–494 https://doi.org/10.1037/a0013589.https://doi.org/10.1037/a0013589.
Burgess Moser, M., & Johnson, S. (2008). The integration of systems and humanistic approaches in Emotionally Focused Therapy for Couples. Person-Centered and Experiential Psychotherapies, 7(4), 262–278. https://doi.org/10.1080/14779757.2008.9688472.https://doi.org/10.1080/14779757.2008.9688472
Farma, K. K. F., Jalili, Z., Zareban, I., & Pour, M. S. (2014). Effect of education on preventive behaviors of breast cancer in female teachers of guidance schools of Zahedan city based on health belief model. Journal of Education and Health Promotion, 3(1), 77. https://doi.org/10.4103/2277–9531.139240.https://doi.org/10.4103/2277–9531.139240
Götze, H., Taubenheim, S., Dietz, A., Lordick, F., & Mehnert‐Theuerkauf, A. (2019). Fear of cancer recurrence across the survivorship trajectory: Results from a survey of adult long‐term cancer survivors. Psycho‐oncology, 28(10), 2033–2041. https://doi.org/10.1002/pon.5188.https://doi.org/10.1002/pon.5188
Guarino, A., Polini, C., Forte, G., Favieri, F., Boncompagni, I., & Casagrande, M. (2020). The effectiveness of psychological treatments in women with breast cancer: A systematic review and meta-analysis. Journal of Clinical Medicine, 9(1), 209–235. https://doi.org/10.3390/jcm9010209.https://doi.org/10.3390/jcm9010209
Hasannezhad Reskati, M., Hosseini, S. H., Alizadeh-Navaei, R., Khosravi, S., & Mirzaian, B. (2020). Effectiveness of Acceptance and Commitment Therapy Management on Self-Differentiation and Fear of Disease Progression in Patients with Breast Cancer. Journal of Babol University of Medical Sciences, 22(1), 110–118. https://doi.org/10.22088/jbums.22.1.110.https://doi.org/10.22088/jbums.22.1.110
Herschbach, P., Berg, P., Dankert, A., Duran, G., Engst-Hastreiter, U., Waadt, S., … & Henrich, G. (2005). Fear of progression in chronic diseases: psychometric properties of the Fear of Progression Questionnaire. Journal of psychosomatic research, 58(6), 505–511. https://doi.org/10.1016/j.jpsychores.2005.02.007.https://doi.org/10.1016/j.jpsychores.2005.02.007
Herschbach, P., Book, K., Dinkel, A., Berg, P., Waadt, S., Duran, G., … & Henrich, G. (2010). Evaluation of two group therapies to reduce fear of progression in cancer patients. Supportive care in cancer, 18(4), 471–479. https://doi.org/10.1007/s00520-009-0696-1.https://doi.org/10.1007/s00520-009-0696-1
Herschbach P., Dinkel A. (2014) Fear of Progression. In Goerling U. (Ed.), Psycho-Oncology. Recent Results in Cancer Research, vol 197 (pp. 11–29). Berlin: Springer. https://doi.org/10.1007/978–3 - 642–40187–9_2.https://doi.org/10.1007/978–3 - 642–40187–9_2.
House, J. S., Landis, K. R., & Umberson, D. (1988). Social relationships and health. Science, 241(4865), 540–545. https://doi.org/10.1126/science.3399889.International Agency for Research on Cancer. (2018, September 12). Latest global cancer data: Cancer burden rises to 18.1 million new cases and 9.6 million cancer deaths in 2018 [Press Release]. WHO. Retrieved on February 1, 2020, from: https://www.who.int/cancer/PRGlobocanFinal.pdfhttps://doi.org/10.1126/science.3399889.Internationalhttps://www.who.int/cancer/PRGlobocanFinal.pdf
Javidi, N. (2014). The effectiveness of emotion-focused couples therapy (EFCT) in improving marital satisfaction and family behavior control. Biannual Journal of Applied Counseling, 3(3), 65–78. https://jac.scu.ac.ir/article_10673.html?lang=enhttps://jac.scu.ac.ir/article_10673.html?lang=en
Javidi, N., Soleimani, A., & Ahmadi Kh, S. M. (2012). The Effectiveness of training of emotion management strategies according to emotionally focused couple therapy (EFT) to increase sexual satisfaction in couples. J Health Psychol, 1(3), 5–18. https://hpj.journals.pnu.ac.ir/article_200.htmlhttps://hpj.journals.pnu.ac.ir/article_200.html
Javidi N, Soleimani A, Ahmadi Kh, Samadzadeh M. (2014). The effectiveness of emotionally focused couples therapy (EFT) to improve communication patterns in couples. J Res Behave Sci, 11(5):402–10. https://doi.org/20.1001.1.17352029.1392.11.5.7.6.https://doi.org/20.1001.1.17352029.1392.11.5.7.6.
Johnson, S. M. (2004). The practice of emotionally focused couple therapy: Creating connection. New York: Brunner-Routledge. https://doi.org/10.4324/9780203017999.https://doi.org/10.4324/9780203017999.
Johnson, S. M. (2008a). Emotionally focused couple therapy. In A. S. Gurman (Ed.), Clinical handbook of couple therapy (4th ed., pp. 107–137). New York: The Guildford Press.
Johnson, S. M. (2008b). Hold me tight: Seven conversations for a lifetime of love. New York: Little, Brown, and Company.
Johnson, S. (2009). The Hold Me Tight program: Facilitator’s guide for small groups. Ontario, Canada: International Center for Excellence in Emotionally Focused Therapy (ICEEFT).
Johnson, S. M., Furrow, J. L., Brubacher, L., Lee, A., Palmer, G., Rheem, K., & Woolley, S. (2013). Becoming an emotionally focused couple therapist: The workbook. Taylor & Francis. https://doi.org/10.4324/9780203955161.https://doi.org/10.4324/9780203955161.
Johnson, S. M., & Greenberg, L. S. (1985a). Differential effects of experiential and problem-solving interventions in resolving marital conflict. Journal of Consulting and Clinical Psychology, 53(2), 175–184. https://doi.org/10.1037//0022–006x.53.2.175.https://doi.org/10.1037//0022–006x.53.2.175
Johnson, S. M., & Greenberg, L. S. (1985b). Emotionally focused couples therapy: An outcome study. Journal of Marital and Family Therapy, 11(3), 313–317. https://doi.org/10.1111/j.1752-0606.1985.tb00624.xhttps://doi.org/10.1111/j.1752-0606.1985.tb00624.x
Kwakkenbos, L., van den Hoogen, F. H., Custers, J., Prins, J., Vonk, M. C., van Lankveld, W. G., … & van den Ende, C. H. (2012). Validity of the Fear of Progression Questionnaire‐Short Form in patients with systemic sclerosis. Arthritis Care & Research, 64(6), 930–934. https://doi.org/10.1002/acr.21618.https://doi.org/10.1002/acr.21618
Lebel, S., Ozakinci, G., Humphris, G., Mutsaers, B., Thewes, B., Prins, J., … & Butow, P. (2016). From the normal response to the clinical problem: definition and clinical features of fear of cancer recurrence. Supportive Care in Cancer, 24(8), 3265–3268. https://doi.org/10.1007/s00520-016-3272-5.https://doi.org/10.1007/s00520-016-3272-5
Li, Q., & Loke, A. Y. (2014). A systematic review of spousal couple‐based intervention studies for couples coping with cancer: Direction for the development of interventions. Psycho‐Oncology, 23(7), 731–739. https://doi.org/10.1002/pon.3535.https://doi.org/10.1002/pon.3535
Lynch, L. E. (2015). Couples coping with cancer: A Hold Me Tight pilot intervention study (Doctoral dissertation, Drexel University). https://doi.org/10.22059/JAPR.2022.318332.643749.https://doi.org/10.22059/JAPR.2022.318332.643749.
Maheu, C., & Galica, J. (2018). The fear of cancer recurrence literature continues to move forward: a review article. Current opinion in supportive and palliative care, 12(1), 40–45. https://doi.org/10.1097/SPC.0000000000000323.https://doi.org/10.1097/SPC.0000000000000323
McLean, L. M., & Nissim, R. (2007). Marital therapy for couples facing advanced cancer: Case review. Palliative & Supportive Care, 5(3), 303–313. https://doi.org/10.1017/s1478951507000466.https://doi.org/10.1017/s1478951507000466
McLean, L. M., Walton, T., Rodin, G., Esplen, M. J., & Jones, J. M. (2011). A couple‐based intervention for patients and caregivers facing end‐stage cancer: Outcomes of a randomized controlled trial. Psycho‐Oncology, 22(1), 28–38. https://doi.org/10.1002/pon.2046.https://doi.org/10.1002/pon.2046.
Mehnert, A., Berg, P., Henrich, G., & Herschbach, P. (2009). Fear of cancer progression and cancer‐related intrusive cognitions in breast cancer survivors. Psycho‐Oncology: Journal of the Psychological, Social and Behavioral Dimensions of Cancer, 18(12), 1273–1280. https://doi.org/10.1002/pon.1481.https://doi.org/10.1002/pon.1481
Mehnert, A., Herschbach, P., Berg, P., Henrich, G., & Koch, U. (2006). Fear of progression in breast cancer patients – validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Zeitschrift fur Psychosomatische Medizin und Psychotherapie, 52(3), 274–288. https://doi.org/10.13109/zptm.2006.52.3.274.https://doi.org/10.13109/zptm.2006.52.3.274
Morgan, M. A., Small, B. J., Donovan, K. A., Overcash, J., & McMillan, S. (2011). Cancer patients with pain: The spouse/partner relationship and quality of life. Cancer Nursing, 34(1), 13–23. https://doi.org/10.1097/NCC.0b013e3181efed43.https://doi.org/10.1097/NCC.0b013e3181efed43.
Nafissi, N., Khayamzadeh, M., Zeinali, Z., Pazooki, D., Hosseini, M., Akbari, M. (2018). Epidemiology and Histopathology of Breast Cancer in Iran versus Other Middle Eastern Countries. Middle East Journal of Cancer, 9(3), 243–251. https://doi.org/10.30476/MEJC.2018.42130.https://doi.org/10.30476/MEJC.2018.42130.
Naughton, M. J., & Weaver, K. E. (2014). Physical and mental health among cancer survivors: considerations for long-term care and quality of life. North Carolina Medical Journal, 75(4), 283–286. https://doi.org/10.18043/ncm.75.4.283.https://doi.org/10.18043/ncm.75.4.283
Noor, S. R., Noor, N., & Haq, M. M. (2016). Breast cancer in Muslim countries: risk reduction strategies. Journal of Advances in Medicine and Medical Research, 16(10), 1–11.
Sabariego, C., Brach, M., Herschbach, P., Berg, P., & Stucki, G. (2011). Cost-effectiveness of cognitive-behavioral group therapy for dysfunctional fear of progression in cancer patients. The European Journal of Health Economics, 12(5), 489–497. https://doi.org/10.1007/s10198–010–0266-y.https://doi.org/10.1007/s10198–010–0266-y
Santos, C. F. (2020). Reflections about the impact of the SARS-COV-2/COVID-19 pandemic on mental health. Brazilian journal of psychiatry, 42, 329–329. https://doi.org/10.1590/1516-4446-2020-0981.https://doi.org/10.1590/1516-4446-2020-0981.
Sharpe, L., Thewes, B., & Butow, P. (2017). Current directions in research and treatment of fear of cancer recurrence. Current opinion in supportive and palliative care, 11(3), 191–196. https://doi.org/10.1097/SPC.0000000000000288.https://doi.org/10.1097/SPC.0000000000000288
Simard, S., Thewes, B., Humphris, G., Dixon, M., Hayden, C., Mireskandari, S., & Ozakinci, G. (2013). Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. Journal of Cancer Survivorship, 7(3), 300–322. https://doi.org/10.1007/s11764–013–0272-z.https://doi.org/10.1007/s11764–013–0272-z
Sun, Y. S., Zhao, Z., Yang, Z. N., Xu, F., Lu, H. J., Zhu, Z. Y., … & Zhu, H. P. (2017). Risk factors and preventions of breast cancer. International Journal of Biological Sciences, 13(11), 1387–1397. https://doi.org/10.7150/ijbs.21635.https://doi.org/10.7150/ijbs.21635
van Helmondt, S. J., van der Lee, M. L., & de Vries, J. (2016). Study protocol of the CAREST trial: a randomized controlled trial on the (cost-) effectiveness of a CBT-based online self-help training for fear of cancer recurrence in women with curatively treated breast cancer. BMC Cancer, 16(1), 1–11. https://doi.org/10.1186/s12885-016-2562-0.https://doi.org/10.1186/s12885-016-2562-0
Wiebe, S. A., & Johnson, S. M. (2016). A review of the research in emotionally focused therapy for couples. Family Process, 55(3), 390–407. https://doi.org/10.1111/famp.12229.https://doi.org/10.1111/famp.12229
Yang, H. C., & Schuler, T. A. (2009). Marital quality and survivorship: slowed recovery for breast cancer patients in distressed relationships. Cancer, 115(1), 217–228. https://doi.org/10.1002/cncr.23964.https://doi.org/10.1002/cncr.23964
Ziner, K. W., Sledge Jr, G. W., Bell, C. J., Johns, S., Miller, K. D., & Champion, V. L. (2012, May). Predicting fear of breast cancer recurrence and self-efficacy in survivors by age at diagnosis. In Oncology Nursing Forum (Vol. 39, No. 3, p. 287–295). NIH Public Access. https://doi.org/10.1188/12.ONF.287–295.https://doi.org/10.1188/12.ONF.287–295