Introduction
Neurogenic bladder patients who use clean intermittent catheterization (CIC) through an abdominal stoma utilize an emptying system that has many shortcomings. Due to a lack of a coordinated bladder contraction for those with emptying issues, bladder evacuation through CIC relies on the hydrostatic pressure from the fluid in the bladder and on external bladder pressures. This gravity-dependent process can result in inadequate emptying of urine, mucus, or other precipitates leading to urinary tract infections (UTIs) and bladder stones.1,2 Small internal catheter diameter further limits drainage speed when relying solely on hydrostatic pressure. Although not quantified in the literature, based on the authors’ expert opinion, many patients have reported that the slow draining and irrigating process has resulted in a decreased quality of life (QoL).
At present, there are no commercially available products aimed at improving bladder emptying for neurogenic bladder patients that use CIC — a population of tens of thousands of people in the United States alone.3 Device solutions exist that are able to individually apply controlled irrigation pressure (eg, wound irrigation devices), individually apply controlled suction pressure (eg, stomach pumps), and are able to interface with catheters (eg, power syringes)4; however, there does not yet seem to be a device that combines all 3 features and is compatible with CIC. Accessories that monitor bladder pressure5 and utilize a pump to aid in drainage have been created, but these devices have not yet been designed to address the irrigation process. As such, there is a need to develop an improved emptying technique that is able to fully drain and irrigate the bladder of both urine and mucus to prevent UTIs and bladder stones while improving QoL for neurogenic bladder patients who use CIC through a catheterizable stoma.
Through a one-year collaboration between a 5-person undergraduate biomedical engineering student design team and client mentors from the affiliated pediatric urology department during the students’ senior engineering capstone design course, solutions to enhance emptying of bladders that require intermittent catheterization were evaluated. This evaluation was done by conducting a patient needs and market analysis, generating design concepts, and building alpha and beta prototypes, called MICath, which were tested through verification and usability testing using a simulated test environment.6
Methods
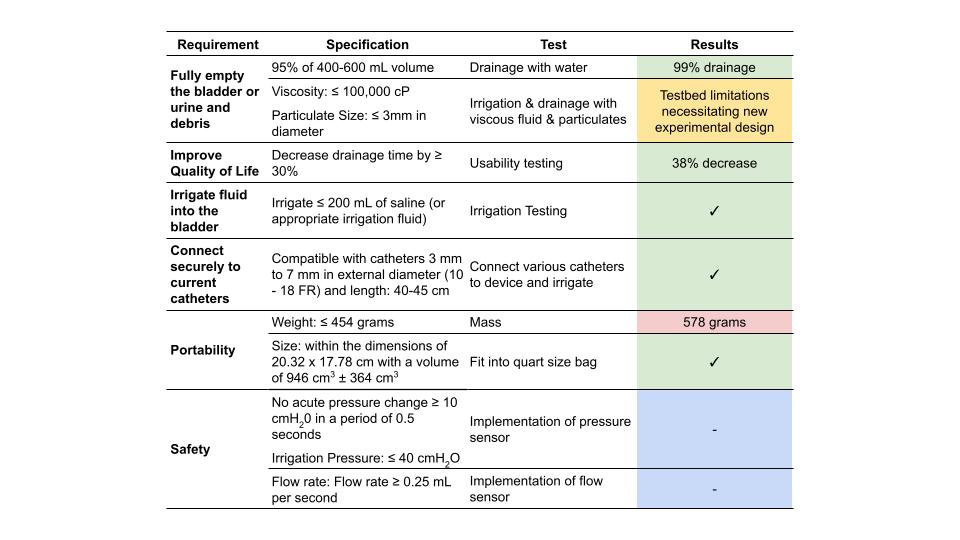
To develop a working prototype, a list of design requirements was developed and categorized to include those that would be feasible to address within the 12-month engineering design course time frame. The design requirements aimed to address the main issues with drainage time and complete emptying while ensuring patient comfort and QoL (Table 1).
Summary of the Verifications Requirements, Tests Conducted, and Their Results
|
Green indicates tests that were passed. Red indicates tests that were failed. Yellow indicates tests that were conditionally passed. Blue indicates requirements to be addressed in future prototypes.
Concept Evaluation
Three different electronic pumps were evaluated for their fluid flow capabilities: a motor pipette pump, a peristaltic pump, and a diaphragm pump. The pumps were evaluated based on 6 different criteria: rate of emptying, control over pressure, ability to provide both suction and irrigation pressure, reusability, portability, and cost. Using a Pugh matrix, an engineering decision-making tool,7 the peristaltic pump was determined to be the most effective pump for our device since it can generate both suction and irrigation pressure while also preventing pump contact with fluid by use of replaceable and easily cleanable tubing.
Phantom Bladder Model
To perform initial verification of the device’s functions, tests were performed against a phantom bladder model. The phantom bladder is modeled by an emptied-out stress ball, which we have previously shown to have high compliance with filling under low pressures,8 as do most medically and surgically optimized neurogenic bladders. The phantom bladder was placed under 5 cm H2O of external pressure to mimic resting abdominal wall pressures, and a catheter was then tunneled and sealed through the phantom bladder 0.5 cm from the bottom to mimic catheterizable channel entry site at the base of the bladder. Phantom stoma site was 16 cm from entry into the bladder.
Verification Tests
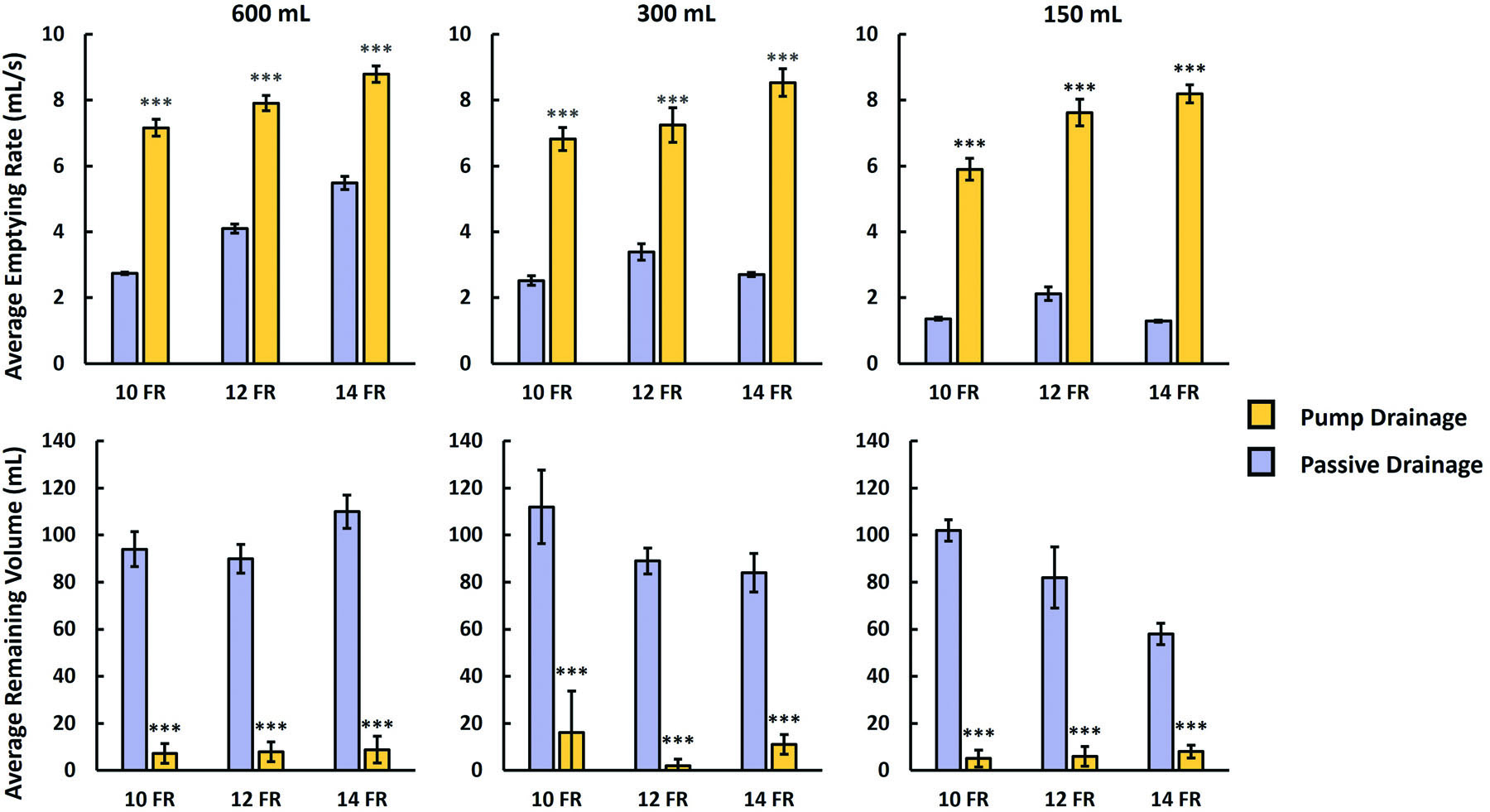
We constructed models for 10, 12, and 14 Fr catheters. Bladder emptying rates and remaining volumes of fluid were tested against phantom bladders filled with 150, 300, or 600 mL of water. Comparisons were made via the catheter either by passive drainage or with aid of the pump. Irrigation was tested by instilling empty bladders with 120 mL of water using a 14 Fr catheter, mixing fluid back and forth 5 times, and then draining the bladder using either a syringe or the pump. Five independent tests were performed for each condition, and Student’s t tests were used to calculate significance between conditions. Emptying efficiency was defined as the fractional percentage of drained volume by starting volume. Preliminary usability testing was also performed to simulate performance of the device in a CIC environment. Eight college student users attached the device to a pre-filled phantom bladder model, the time for suction and irrigation was measured, and user feedback was collected, comparing the performance of the pump and syringe. In the feedback survey, the users were asked to rate the ease of use of the pump compared to the syringe on a 1 to 5 scale with 1 being very easy to use and 5 being very difficult.
Results
The final design of the device, dubbed the MICath, consists of a compact all-in-one pump that improves bi-directional fluid movement during CIC in a phantom bladder model. An overview of the verification tests conducted and results of the MICath pump are highlighted in Table 1.
Mechanical Specifications
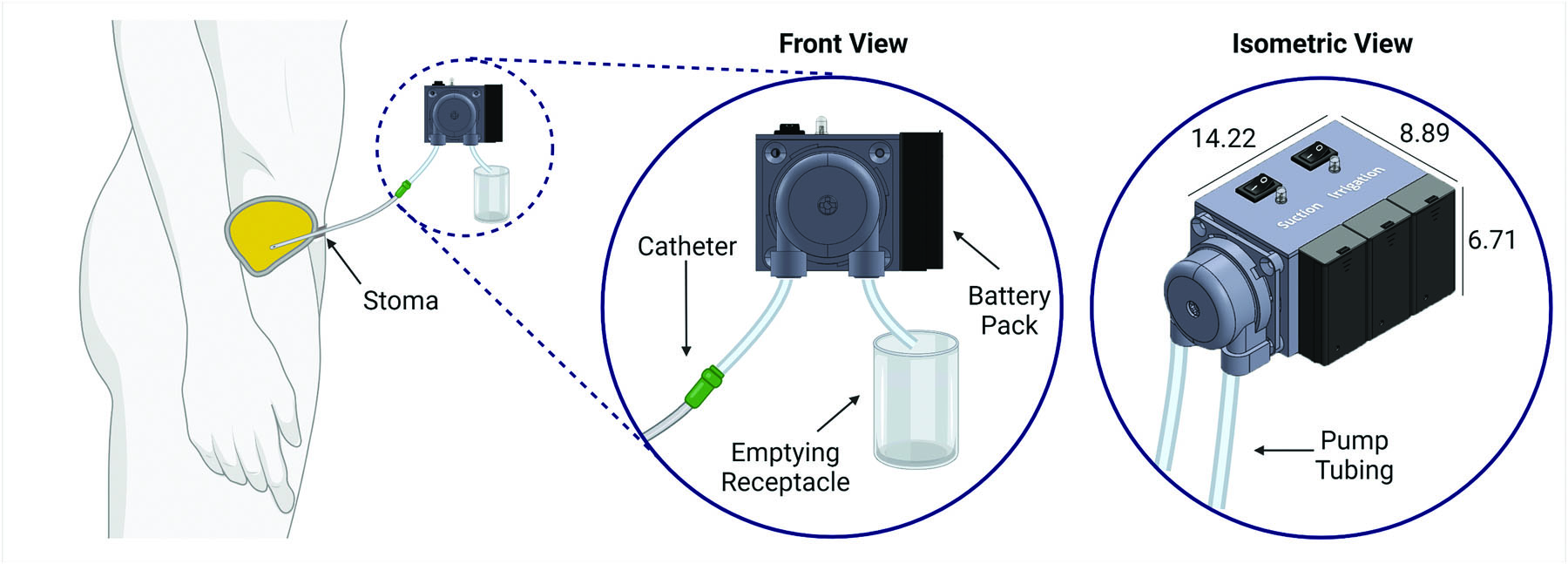
The mechanical components of the device were assembled using a 3D-printed housing, an ANKO A200 peristaltic pump (ANKO Products, Bradenton, FL) with ¼ in internal diameter × ⅜ in outer diameter latex tubing. The ANKO A200 pump was selected due to its high flow rates up to 10 mL/s and easy attachment of tubing. The 3D-printed box was designed using SolidWorks (Dassault Systèmes, Vélizy-Villacoublay, France) with a center hole for the pump motor and threaded M4 screw holes to secure the peristaltic pump head to the outside of the box. Four pegs were positioned at the base of the box for the solderable breadboard and circuit components to be secured and grounded to the plastic housing. The box was printed using a Form 3 SLA printer and clear resin (Formlabs, Somerville, MA). When fully assembled, the dimensions were 14.22 × 8.89 × 6.71 cm, as seen in Figure 1.
Electrical Specifications
An Arduino Nano (Arduino, Turin, Italy) was used to control the main components of our system. The Nano powered and controlled 2 LEDs and a buzzer for patient feedback on the device operation status and received input from 2 rocker switches that the patient uses to control pump direction. A L293D H-bridge controller (PIXNOR, Shenzhen City, China) was used to control the direction and speed of the pump. The Nano also monitored the current through the pump and was capable of automatic shutdown if the current passed a threshold current of 390 mA, which is set to 30% above the expected load on the pump. A high current load suggested (although not formally tested) the pump was under high pressure, either due to a kink in the tubing or due to sucking on the phantom bladder wall. Three 9V rechargeable lithium batteries were used to power the system, and the pump could be operated continuously for roughly one hour before recharging was required.
Verification Testing
Testing results showed that for all bladder volumes and catheter sizes, the pump had >98% emptying efficiency and drained between 1.6 and 6.3 times faster than passive drainage. In general, the pump emptying rate continually increased with catheter gauge, and emptying rate increased as initial bladder volume increased, both as expected (Figure 2). The largest improvements in drainage rate between pump drainage and passive drainage were found in 10 Fr catheters and between small bladder volumes. Across all catheter sizes, the pump vastly outperforms passive drainage with regard to the amount of fluid able to be drained from the bladder. With regard to irrigation testing, instilling 120 mL into bladders, performing 5 back-and-forth mixes, and subsequent draining took a mean time of 76.2 ± 3.56 seconds using the pump, compared to 107.4 ± 4.83 seconds using a syringe (p<0.001). During verification testing, unintended automatic shutdown secondary to high current load did not occur.
Usability testing indicated that the pump had a significant decrease in the total time on task when compared to the syringe irrigation method. Users were able to complete the usability tasks 38% faster from initiation of first catheter connection to final disconnection and storage of the pump compared to the syringe technique (pump: 138 ± 32 seconds; syringe: 224 ± 51 seconds; p=0.001). The users rated the pump as 3 points easier to use on a 5-point scale, where 1 is the easiest to use and 5 is the most difficult, compared to the syringe (median score: pump 1; syringe 4).
Discussion
From this work, we were able to successfully develop a working prototype that improved drainage and irrigation efficiency compared to the current methods. The methodologies utilized in the design of this device could be applied to improve QoL of neurogenic bladder patients by decreasing UTI and bladder stone incidence because of higher emptying efficiency and better patient compliance as a result of decreased drainage times. This hypothesis will need to be tested in patient-based studies. This also has the theoretical benefit of improved irrigation abilities for those patients with poor hand dexterity because the pump does not require device disconnection between irrigation and suction as does the syringe method.
Improving the device form factor, by decreasing size and optimizing ease of use, should further improve usability. A final version of the product would ideally be able to be operated and fit in one hand. Another potential improvement is a safety shutoff mechanism to ensure the device complies with bladder safety standards. Inline flow and pressure sensors along with monitoring of the pump electrical load would help to determine an automatic shutoff threshold for the device before it begins to apply suction pressure to the bladder wall. These safety features would also be able to regulate irrigation pressure. An emergency shutoff button would be designed to be quickly accessible for pump malfunction.
Product testing with college-aged students without prior self-catheterization experience decreases the significance of the usability testing; however, it does serve to demonstrate that the device can undergo repeated use without malfunctioning. Patient validation will be required prior to commercialization, which will be integrated once the device goes through more formal safety testing in subsequent prototypes. Furthermore, additional testing of the pump in animal or cadaver bladders may be required prior to patient introduction. This would allow stress analysis on the bladder wall during suction and irrigation. By establishing this initial groundwork for the pump’s functionality, these proposed features can be more easily implemented in future iterations.
Conclusion
The MICath pump improves bladder emptying by increasing flow rate, decreasing residual volume, and increasing ease of use in a phantom bladder model. This project demonstrates both the feasibility of a catheter accessory device to improve patient QoL and the ability for understudied clinical problems to be addressed through collaboration between capstone engineering design teams and medical school affiliates.
References
1 Kisku S, Sen S, Karl S, Mathai J, Thomas RJ, Barla R. Bladder calculi in the augmented bladder: a follow-up study of 160 children and adolescents. J Pediatr Urol. 2015; 11(2):66.e1–66.e6. doi:10.1016/j.jpurol.2014.12.00310.1016/j.jpurol.2014.12.003
2 Husmann DA. Lessons learned from the management of adults who have undergone augmentation for spina bifida and bladder exstrophy: incidence and management of the non-lethal complications of bladder augmentation. Int J Urol. 2018; 25(2):94–101. doi:10.1111/iju.1341710.1111/iju.13417
3 Ginsberg D. The epidemiology and pathophysiology of neurogenic bladder. Am J Manag Care. 2013; 19(10):191–196. https://www.ajmc.com/view/ace012_jul13_ngb_ginsberg1_s191https://www.ajmc.com/view/ace012_jul13_ngb_ginsberg1_s191
4 Ducksoo K, Smith JL, Crunkleton JA, inventors. A self-contained power assisted syringe. U.S. Patent No. US2011196232A1. April 29, 2014.
5 Cooper CS, Steinberg RL, Thomas LJ, et al. Neurogenic bladder monitoring using the cystomanometer and cystoelastometer. J Pediatr Urol. 2020; 16(2):182–188. doi:10.1016/j.jpurol.2019.12.01410.1016/j.jpurol.2019.12.014
6 Sack BS, Elizondo RA, Huang GO, et al. Pediatric medical device development by surgeons via capstone engineering design programs. J Pediatr Surg. 2018; 53(3):493–498. doi:10.1016/j.jpedsurg.2017.01.06710.1016/j.jpedsurg.2017.01.067
7 S. Pugh. Concept selection: a method that works. In: Proceedings of International Conference on Engineering Design. Heurista, Zürich; 1981:497–506.
8 Kalayeh K, Fowlkes JB, Claflin J, Fabiilli ML, Schultz WW, Sack BS. Benchtop bladder phantom pressure estimation using ultrasound contrast agents. Poster presented at: American Urological Association Annual Meeting; September 10–13, 2021; Virtual.