Introduction
Among 11 industrialized nations, the United States has the highest maternal mortality rate at 17.4 per 100,000 live births.1 Adverse birth events, including cesarean sections, are often implicated in increased maternal mortality from birth, while other maternal behaviors, such as breastfeeding, have been shown to decrease maternal morbidity and mortality.2,3 Continuous support during labor has been shown to reduce the likelihood of these adverse birth events.4 Doulas, uniquely trained nonmedical support professionals who can provide this continuous support to pregnant women during labor, have been shown to reduce rates of these adverse birth outcomes and increase rates of breastfeeding.4,5 The benefits of doula care are explored in this study through a retrospective analysis of a national dataset of doula-supported births occurring between 2000 and 2012 in the United States.
Prior to birth, the scope of doula care often involves psychosocial support, childbirth education, and information on maintaining a healthy pregnancy. During labor and childbirth, doulas provide physical, emotional, and informational support.6 Evidence shows that continuous labor support is highly effective and is associated with the likelihood of shorter labor, spontaneous vaginal birth, fewer instrumental births, decreased rates of cesarean births, and increases in both breastfeeding initiation and duration of time.7 Although partners, family members, friends, or healthcare professionals can provide continuous support, research has shown that compared to these caregivers, doulas are more likely to receive a higher rating from birthing women for their supportive care.8
From 2005 to 2012, the percentage of women who used a doula doubled (from 3% to 6%).8
Professional societies recognize that the continuous presence of doulas can help improve obstetric outcomes.8,9 Benefits found in randomized trials include shortened labor, decreased need for analgesia, fewer operative deliveries, and fewer reports of dissatisfaction with the experience of labor.10 Several states provide Medicaid reimbursement for doula care (eg, Minnesota, Oregon, New York), and others have recently introduced legislation for Medicaid coverage of doula care.11 Still, an estimated 40% or more of women are unaware of doula care and the potential support doulas can provide.12
One particular professional doula certifying organization that has been collecting birth data is Doulas of North America (DONA) International. DONA International promotes perinatal support for birthing women and their families.6 The organization operates as a nonprofit with the primary goal of providing evidence-based training and certification for a globally diverse population of doulas. DONA training is comprehensive; the program requires the in-person completion of an approved doula workshop (minimum 16 hours), an accredited childbirth education series (minimum 12 hours), a basic breastfeeding workshop, and reading of at least 8 texts from the Birth Doula Required Reading List. Doulas must pass a written self-assessment and provide a total minimum of 15 hours of continuous in-person labor support throughout 3 births, only one of which can be a cesarean birth. However, certification is not required for membership in DONA International.
While there have been several studies or reports that evaluate doula programs and their outcomes, we are unaware of any other descriptive studies that have analyzed such a large birth dataset collected by a doula certifying organization.13–18 DONA International has one of the largest previously unanalyzed datasets about doulas and the women they support. The purpose of this article is to provide descriptive information about the characteristics related to doulas, doula-supported women, childbirth settings and providers, and obstetric outcomes from a national sample of doula-supported births using data collected by DONA International between 2000 and 2012. This is the largest study to date examining the effects of doula care for childbearing women and is one of the few to report on outcomes from a national sample.
Methods
Data and Study Population
We undertook a primary data analysis using data from DONA International. The population was composed of women who received doula care provided by members of DONA International. Data on DONA doula-supported births came from DONA’s Birth Doula Data Collection Form. Data was submitted by DONA International doulas, including certified doulas, certification candidates, and non-certified doulas. Doulas used one form per birth and either mailed or faxed their completed form to DONA International, Chicago, Illinois. The data collection form has 15 categories, including birthing demographics, place of birth and type of healthcare provider, pregnancy and labor and birth information, and infant outcomes. It includes the name and zip code of the doula, but there is no identifiable information about birthing women. Doulas are not required to complete Birth Doula Data Collection Forms.
DONA volunteers entered the data from the Birth Doula Data Collection Forms into SPSS statistical software to create a dataset (N=33,247). The authors of this article verified the accuracy of the data entry and analyzed a portion of the DONA dataset about doula-supported US births.
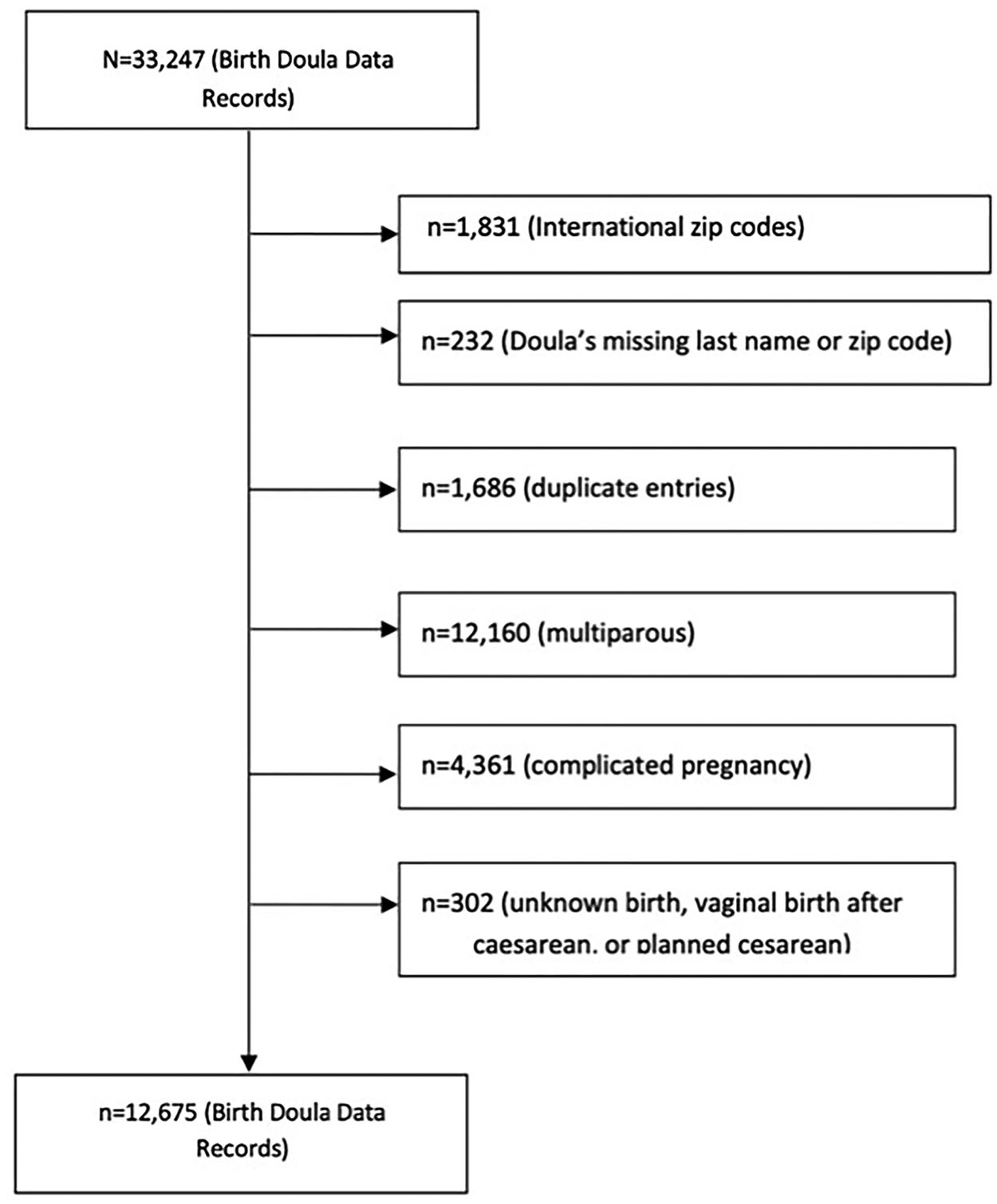
The following exclusion criteria were applied: (1) international zip codes (n=1831); (2) missing doula last names and/or zip codes (n=232); and (3) duplicate entries (n=1686). Further exclusion criteria were applied to obtain a sample of birthing individuals: multiparous birth (n=12,160), complicated pregnancy (defined on the collection form as the presence of gestational diabetes, pregnancy-induced hypertension, gestation <38 weeks or >42 weeks, high-risk, and “other” reasons) (n=4361), and method of birth (unknown, vaginal birth after cesarean, and planned cesarean) (n=302). After exclusion and inclusion criteria were applied, 20,572 observations were removed from the dataset (Figure 1).
Delimitation began with the number of DONA International Birth Doula Data Collection Forms. Final analyses were limited to women who gave birth with a DONA International doula in the United States.
Variables
We derived variables from the DONA Birth Doula Data Collection Form. Primary outcomes of interest were characteristics related to doulas (source of doula client referrals, payment source for doula services), doula-supported birthing women (mother’s age, childbirth education, breastfeeding initiation), childbirth settings and providers, and obstetric outcomes (induction, Pitocin or other augmentation, artificial rupture of membranes (AROM), intravenous (IV) fluids, epidural administration, and method of birth). To examine the prevalence of the characteristics mentioned above, we applied an urban-rural classification to illuminate the subtle underlying geographic or demographic patterns.
Analysis
Descriptive statistics were performed to examine the number of doula-assisted births per 10,000 births by state. We calculated mean maternal age and standard deviation (SD), percentage of all births for characteristics related to doulas, doula-supported birthing women, childbirth settings and providers, and obstetric outcomes. We used t tests or Pearson’s chi-squared test (X2) to compare urban to rural doula-supported births. We used rural-urban commuting area codes to derive urban versus rural residence based on zip code.19 Analyses were carried out using Stata version 13.0 (StataCorp). Missing data occurred in less than 3% of outcome variables. Therefore, we used complete case analysis to deal with missing data.
Results
The study sample included 12,675 observations. Table 1 presents descriptive characteristics related to doulas, doula-supported birthing women, childbirth settings and providers, and obstetric outcomes and by urban-rural classification. Regarding birthing women, our findings indicate the mean maternal age was 28.6 years (SD ± 6.22).
Descriptive characteristics related to doulas, doula-supported birthing women, childbirth settings/providers, and obstetric outcomes by urban and rural areas: 2000–2012
Characteristics |
All births (%) (n=12,675) |
Births in urban areas (%) (n=12,079) |
Births in rural areas (%) (n=596) |
|---|---|---|---|
Doulas |
|||
| Source of referrals to doula | |||
| Hospital | 4743 (37.4) | 4681 (38.8)*** | 62 (10.4) |
| DONA International | 1059 (8.4) | 1021 (8.5) | 38 (6.4) |
| Other | 6700 (52.9) | 6214 (51.4) | 486 (81.5) |
| Missing | 173 (1.4) | 163 (1.4) | 10 (1.7) |
| Payment source for doula services | |||
| Self-pay | 6300 (49.7) | 5934 (49.1)*** | 366 (61.4) |
| Hospital | 4416 (34.8) | 4309 (35.7) | 107 (18.0) |
| Third-party reimbursement | 166 (1.3) | 160 (1.3) | 6 (1.0) |
| Volunteer | 1343 (10.6) | 1255 (10.4) | 88 (14.8) |
| Other | 135 (1.1) | 125 (1.0) | 10 (1.7) |
| Missing | 315 (2.5) | 296 (2.5) | 19 (3.2) |
Doula-supported birthing women |
|||
Maternal age, mean (SD) |
28.6 (±6.22) |
28.6 (±6.19) |
28.0 (±6.76) |
| Childbirth education | |||
| Yes | 9332 (73.6) | 8844 (73.2)*** | 488 (81.9) |
| No | 3088 (24.4) | 2987 (24.7) | 101 (17.0) |
| Missing | 255 (2.0) | 248 (2.1) | 7 (1.2) |
| Breastfeeding initiation | |||
| Yes | 10,061 (79.4) | 9574 (79.3) | 487 (81.7) |
| No | 2552 (20.1) | 2449 (20.3) | 103 (17.3) |
| Missing | 62 (0.5) | 56 (0.5) | 6 (1.0) |
Childbirth settings and providers |
|||
| Place of birth | |||
| Hospital | 11,258 (88.8) | 10,753 (89.0)*** | 505 (84.7) |
| Birth center | 1028 (8.1) | 974 (8.1) | 54 (9.1) |
| Home | 327 (2.6) | 296 (2.5) | 31 (5.2) |
| Other | 6 (0.1) | 6 (0.1) | 0 (0.0) |
| Missing | 56 (0.4) | 50 (0.4) | 6 (1.0) |
| Type of healthcare provider | |||
| OB-GYN | 8678 (68.5) | 8369 (69.3)*** | 309 (51.9) |
| Midwife | 2704 (21.3) | 2558 (21.2) | 146 (24.5) |
| Family practitioner | 691 (5.5) | 584 (4.8) | 107 (18.0) |
| Combination | 535 (4.2) | 502 (4.2) | 33 (5.5) |
| Other | 1 (0.0) | 1 (0.0) | 0 (0.0) |
| Missing | 66 (0.5) | 65 (0.5) | 1 (0.2) |
Obstetric outcomes (labor/birth) |
|||
| Induction | |||
| Yes | 2936 (23.2) | 2827 (23.4) | 109 (18.3) |
| No | 9739 (76.8) | 9252 (76.6) | 487 (81.7) |
| AROM | |||
| Yes | 4581 (36.1) | 4370 (36.2) | 211 (35.4) |
| No | 8072 (63.7) | 7688 (63.7) | 384 (64.4) |
| Missing | 22 (0.2) | 21 (0.2) | 1 (0.2) |
| Pitocin or other augmentation | |||
| Yes | 4413 (34.8) | 4224 (35.0) | 189 (31.7) |
| No | 8262 (65.2) | 7855 (65.0) | 407 (68.3) |
| Intravenous fluids | |||
| Yes | 3874 (30.6) | 3718 (30.8)* | 156 (26.2) |
| No | 8793 (69.4) | 8353 (69.2) | 440 (73.8) |
| Missing | 8 (0.1) | 8 (0.1) | 0 (0.0) |
| Epidural administration | |||
| Before 5 cm | 2973 (23.5) | 2898 (24.0)* | 75 (12.6) |
| After 5 cm | 3662 (28.9) | 3533 (29.3) | 129 (21.6) |
| No epidural | 6040 (47.7) | 5648 (46.8) | 392 (65.8) |
| Method of birth | |||
| Spontaneous vaginal | 9283 (73.2) | 8846 (73.2) | 437 (73.3) |
| Unplanned cesarean | 2306 (18.2) | 2193 (18.2) | 113 (19.0) |
| Forceps/vacuum | 1086 (8.6) | 1040 (8.6) | 46 (7.7) |
* p<0.05,
** p<0.01,
*** p<0.001.
Significance of t tests or Pearson’s chi-square tests comparing urban to rural doula-assisted births:
Doulas reported that, overall, during labor and birth, less than half of the women they supported received an obstetric intervention (induction (23.2%), AROM (36.3%), Pitocin augmentation (34.8%), or IV fluids (30.6%)), with the exception of an epidural. About half (52.4%) of birthing women received an epidural either before 5 cm dilation (23.5%) or after (28.9%). Results show that the vast majority (73.2%) of all doula-supported women birthed by spontaneous vaginal birth. Doulas reported that fewer than 1 in 5 (18.2%) women birthed by unplanned cesarean.
Doulas also reported that, overall, nearly 3 out of 4 (73.2%) women had some form of childbirth preparation instruction. When asked if the birthing women they supported initiated breastfeeding after birth, overall, doulas indicated that, on average, over three-quarters (79.4%) had. For the entire sample, doulas reported the most common childbirth setting was in a hospital (88.8%), and the majority of birthing women (68.5%) were attended by an obstetrician/gynecologist, followed by midwives (21.3%) and family practitioners (5.5%). Approximately 10% of doula-assisted births occurred in birth centers or at home with a midwife or family practitioner.
Doulas reported that out of all birthing women, fewer than 1 in 10 found them through DONA International. Information regarding the source of referrals to doulas suggests that over half (52.9%) of birthing women found a DONA-member doula from a source other than a hospital system or DONA International, followed by a hospital system (37.4%). When asked about the source of payment for their services, doulas reported that, overall, half (49.7%) of birthing women they supported were self-pay clients. Few doulas (1.3%) received third-party reimbursements for their paraprofessional services.
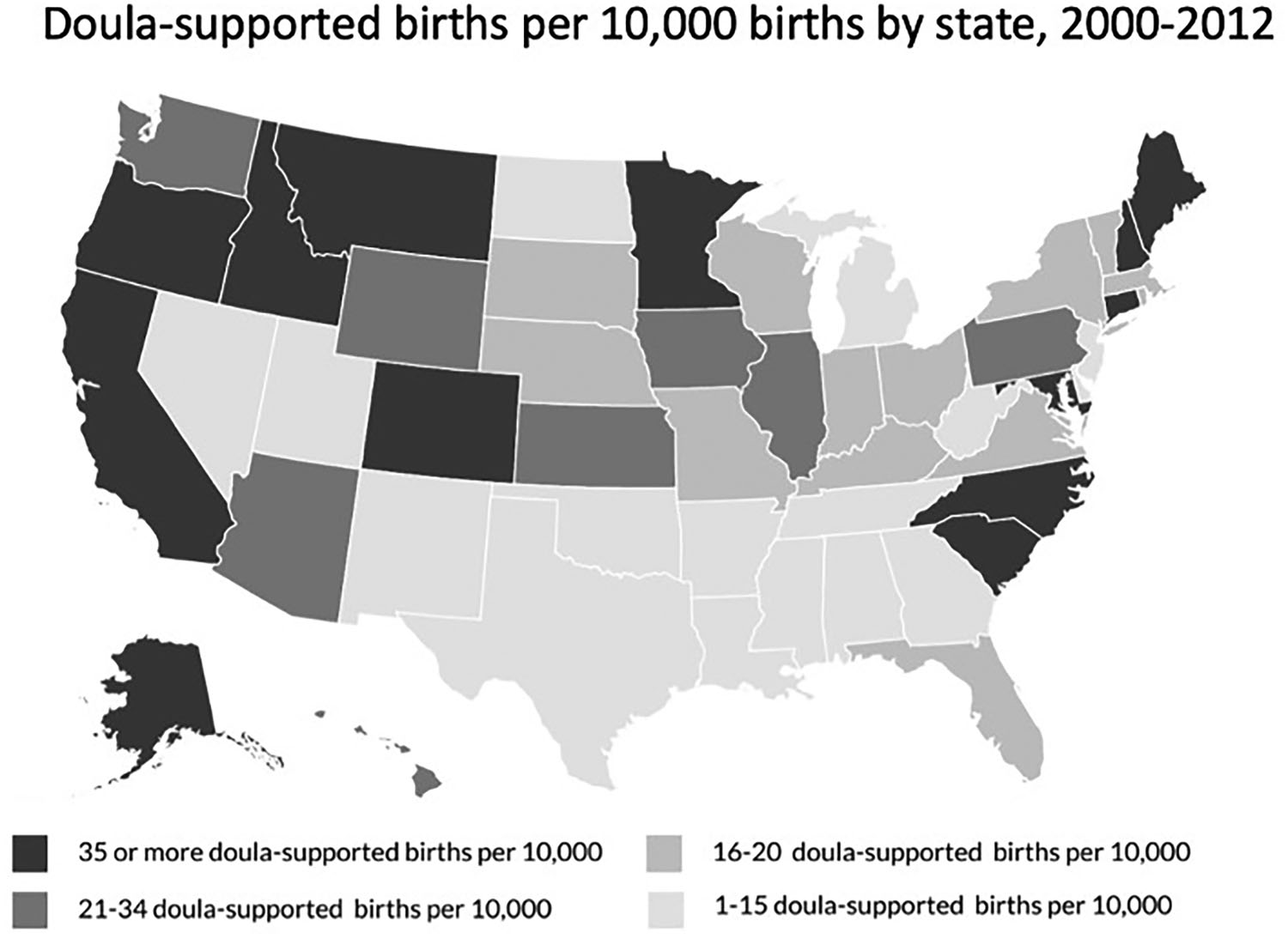
Results suggest that the vast majority (95.3%) of doula-supported births in the sample occurred in urban areas of the United States and in states on both coasts, plus Colorado (Figure 2). (See Appendix for rates of doula-supported births by state.)
Compared to urban birthing women, a significantly higher proportion of rural birthing women received a referral to a doula through an “other” source (81.5% vs 51.4%, respectively; p<0.001) and paid for doula services out of pocket (61.4% vs 49.1%, respectively; p<0.001).
Compared to urban women, a significantly higher proportion of rural women received some form of childbirth education from any source as reported by the doulas who were involved in their birth (73.2% vs 81.9%, respectively; p<0.001). Rural women were also more likely than urban women to give birth in a birth center (9.1% vs 8.1%, respectively; p<0.001) and to have a birth attended by a midwife (24.5% vs 21.2%, respectively; p<0.001). They were more than twice as likely as urban women to give birth at home (5.2% vs 2.5%, respectively; p<0.001) and more than 3 times as likely to be attended by a family practitioner (18.0% vs 4.8%, respectively; p<0.001). By comparison, urban rather than rural women were more likely to receive IV fluids (30.8% vs 26.2%, respectively; p<0.05) and twice as likely to receive an epidural before 5 cm dilation (24.0% vs 12.6%, respectively; p<0.05).
Discussion
This study provides descriptive information from the largest sample to date of doula-supported births in the United States from 2000 to 2012. Similar to a descriptive analysis of doula support among a national sample of adolescent births (n=1892), our findings also found that, overall, women with doula-supported births experienced better birth outcomes compared to women in the general population.6
Some Labor Interventions Reduced With Doula Care
In this analysis of a national sample of doula-supported births, women experienced lower rates of certain interventions compared to national statistics for deliveries in the United States during the same time period. Compared to the average overall epidural rate (65.5%) in the general population for all births (2004 through 2012, years of available data), the rate in the sample (52.3%) was lower.20 While there is controversy over whether epidurals increase the risk of cesarean births, there is evidence that they can lead to an increased likelihood of other medical interventions.21–23 Additionally, the rates of AROM have been increasing over time (34.0% in 2010), while the analysis of the sample suggests that only about 1 in 4 doula-supported birthing women had this intervention.24 The reduced rates of these interventions could be due to a variety of factors, including the continuous support provided by the doulas as well as education on a variety of coping methods for pain.
The United States has a high cesarean birth rate of about 1 in 3 births.25 Compared to the low-risk cesarean birth rate in the general population, the cesarean rate was lower in the sample (26.0% vs 18.2%, respectively) during the same period.26 The lower rate is consistent with evidence from previous research that continuous labor support (ie, a doula) is associated with a decrease in the likelihood of cesarean births.7,10 This could be secondary to the increased advocacy that doulas provide to their patients when communicating with the medical team or that those with doula-supported births had higher rates of child education classes prior to birth.
The failure of intravenous synthetic oxytocin infusion for the treatment of labor arrest is the leading indication for primary cesarean births, making up one-third of all cesarean births in the United States.27 Before 2005, data regarding labor augmentation was not reported in the National Vital Statistics; therefore, a comparison to the sample rate (34%) in this study was not possible. However, it can be inferred that this rate may be higher in the sample given the lower cesarean rates, which supports the American College of Obstetricians and Gynecologists’ (ACOG) recommendation to attempt synthetic oxytocin infusion prior to cesarean section for arrest of labor.28 The rate of forceps/vacuum birth in the sample (8.6%) was twice that as for the general population of all births (4.74%) for the same period.29 The percentage of instrumental births was 9.0% or more before 1998, but as the cesarean rate increased in the general population, the percentage of instrumental births decreased.29
Compared to the average induction rate in the general US population for all births during the same period as the sample, the sample’s induction rate did not differ (23.3% vs 23.2%).30 Underreporting of widespread hospital induction practices in the United States might explain why the induction rates in both the general US population and in the doula-supported population are similar.
Breastfeeding Rates Stable Among Mothers Who Receive Doula Care
While breastfeeding rates in the United States have risen in recent years and are now stabilized around 80%, there is an indication that doula care supports near-universal breastfeeding initiation, especially for underserved women.31 Given this additional encouragement and likely additional education, the sample shows that 8 out of 10 doula-supported mothers did initiate breastfeeding after giving birth, which is similar to the national rate.31
Referrals and Insurance Coverage Lacking for Doula Care
Despite the demonstrated benefits of doula care, the majority (52.9%) of doulas in the sample reported that the women they supported during birth were referred through means other than a hospital or DONA International. Known referral sources are likely associated with friends, family members, childbirth educators, prenatal practices, organizations, and/or forms of media. These data suggest a heightened need for hospitals and obstetricians to provide more information about doulas to their patients.
The majority (49.7%) of doulas reported compensation through self-pay clients, and a small minority (1.3%) reported third-party reimbursement. Similarly, a 2002 study found that the majority (80%) of doulas reported self-pay clients, and a minority (10%) reported third-party reimbursement.9 The high rate of doulas reporting compensation through self-pay, rather than by third-party reimbursement, suggests there may be a lack of insurance coverage for doula services. Insurance coverage plans vary by state. Twenty-one states had ≥21 doula-supported births per 10,000 births, while the remaining states had ≤20 doula-supported births per 10,000 births. Overall, this suggests that lack of state insurance coverage of doula care may be a barrier to use of a doula during birth.
More Doula Births in Urban Areas
We observed that certain regions of the country might have higher rates of doula usage. Furthermore, we noted that births by rural women were less likely to be attended by an obstetrician/gynecologist, likely reflective of the shortage of obstetricians/gynecologists in rural areas and lack of hospitals in those regions that take obstetric patients.32,33 There are significantly higher rates of doula-supported births in urban areas, suggesting that there is potentially a heightened need for doula services in rural areas. Given that insurance coverage is a likely barrier to seeking doula services, and because Medicaid pays for nearly half of all rural births, insurance coverage of doula-supported births would likely be able to reduce this limitation in the rural population.34
Limitations
This study had several methodological limitations. Because there was no control group, meaningful conclusions about the impact of doula-supported care during labor and childbirth were not possible. Information about doula-supported births came from only one doula certifying organization; therefore, trends over time given the voluntary sample are reflective only of what DONA data were available. Although doulas across the United States received the same type of comprehensive training, we could not account for hospital practice variations that might have impacted obstetric care interventions. Additionally, doula training courses are cost prohibitive for many, especially certification and additional expenses associated with breastfeeding classes, reading materials, and organization membership, such that many of the doulas contributing to these data were likely from socioeconomically stable backgrounds.
As noted earlier, reporting births using the Birth Doula Data Collection Form is voluntary. We did not know how many doula-supported births went unreported and cannot know whether there were differences in outcomes between doulas who reported and those who did not report births. Information on the data collection form relied on the self-report of doulas.
Although we had information about maternal race, we did not have information about maternal ethnicity, educational attainment, insurance type, or prenatal care, which hampered our ability to assess disparities in subgroups of the sample population.
We were unable to assess how racially and ethnically diverse women have access to doula services. Extant literature suggests that increased access to doula care, especially in underserved communities, can improve a range of health outcomes for mothers and infants. For example, continuous labor support is especially vital for women of color. Studies have shown that Black women in the general population experience higher rates of pre-term birth, cesarean birth, low birth weight infants, and infant mortality.18 These outcomes have been ameliorated with doula-supported care.18,35 Evidence also suggests that doula support may lower maternal stress and enhance women’s self-efficacy regarding their pregnancy and the ability to manage labor.4,7,13 Given that racial concordance is known to impact health outcomes with Black patients citing poorer communication, information-giving, patient participation, and participatory decision-making than White patients, this study does not adequately cover different races and socioeconomic backgrounds.36,37
Conclusion
The DONA International birth doula dataset is the largest in the United States on the continuous doula care for women during childbirth. Our analysis strengthens the evidence of what is currently known about the benefits of continuous support and why doula care is effective.
Doulas play an increasingly important role as unique members of maternity care teams. Yet despite the recognition of the well-established benefits and absence of identified harms of doula services by professional organizations, doula care is underutilized in the United States. This study suggests there is a need for increased referrals for and insurance coverage of doula services and for doula services in rural areas.
References
1 Douthard RA, Martin IK, Chapple-McGruder T, Langer A, Chang S. U.S. maternal mortality within a global context: historical trends, current state, and future directions. J Womens Health. 2021; 30(2):168–177. doi:10.1089/jwh.2020.886310.1089/jwh.2020.8863
2 Deneux-Tharaux C, Carmona E, Bouvier-Colle M-H, Bréart G. Postpartum maternal mortality and cesarean delivery. Obstet Gynecol. 2006; 108(3 Pt 1):541–548. doi:10.1097/01.AOG.0000233154.62729.2410.1097/01.AOG.0000233154.62729.24
3 Chowdhury R, Sinha B, Sankar MJ, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015; 104(467):96–113. doi:10.1111/apa.1310210.1111/apa.13102
4 Gruber KJ, Cupito SH, Dobson CF. Impact of doulas on healthy birth outcomes. J Perinat Educ. 2013; 22(1):49–58. doi:10.1891/1058-1243.22.1.4910.1891/1058-1243.22.1.49
5 Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017; 7(7):CD003766. doi:10.1002/14651858.CD003766.pub610.1002/14651858.CD003766.pub6
6 Everson CL, Cheyney M, Bovbjerg ML. Outcomes of care for 1,892 doula-supported adolescent births in the United States: the DONA International data project, 2000 to 2013. J Perinat Educ. 2018; 27(3):135–147. doi:10.1891/1058-1243.27.3.13510.1891/1058-1243.27.3.135
7 Hodnett ED, Gates S, Hofmeyr GJ, Sakala C. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2012; 10:CD003766. doi:10.1002/14651858.CD003766.pub410.1002/14651858.CD003766.pub4
8 Declercq ER, Sakala C, Corry MP, Applebaum S. Listening to Mothers II: report of the second national U.S. survey of women’s childbearing experiences. J Perinat Educ. 2007; 16(4):9–14. doi:10.1624/105812407X24476910.1624/105812407X244769
9 Lantz PM, Low LK, Varkey S, Watson RL. Doulas as childbirth paraprofessionals: results from a national survey. Womens Health Issues. 2005; 15(3):109–116. doi:10.1016/j.whi.2005.01.00210.1016/j.whi.2005.01.002
10 ACOG Committee Opinion no. 766: approaches to limit intervention during labor and birth. Obstet Gynecol. 2019; 133(2):e164-e173. doi:10.1097/AOG.000000000000307410.1097/AOG.0000000000003074
11 Collier A-RY, Molina RL. Maternal mortality in the United States: updates on trends, causes, and solutions. Neoreviews. 2019; 20(10):e561-e574. doi:10.1542/neo.20-10-e56110.1542/neo.20-10-e561
12 Kozhimannil KB, Attanasio LB, Jou J, Joarnt LK, Johnson PJ, Gjerdingen DK. Potential benefits of increased access to doula support during childbirth. Am J Manag Care. 2014; 20(8):e340–352.
13 Kozhimannil KB, Hardeman RR, Attanasio LB, Blauer-Peterson C, O’Brien M. Doula care, birth outcomes, and costs among Medicaid beneficiaries. Am J Public Health. 2013; 103(4):e113-e121. doi:10.2105/AJPH.2012.30120110.2105/AJPH.2012.301201
14 Kozhimannil KB, Attanasio LB, Hardeman RR, O’Brien M. Doula care supports near-universal breastfeeding initiation among diverse, low-income women. J Midwifery Womens Health. 2013; 58(4):378–382. doi:10.1111/jmwh.1206510.1111/jmwh.12065
15 Lanning RK, Klaman SL. Evaluation of an innovative, hospital-based volunteer doula program. J Obstet Gynecol Neonatal Nurs. 2019; 48(6):654–663. doi:10.1016/j.jogn.2019.08.00410.1016/j.jogn.2019.08.004
16 Mottl-Santiago J, Walker C, Ewan J, Vragovic O, Winder S, Stubblefield P. A hospital-based doula program and childbirth outcomes in an urban, multicultural setting. Matern Child Health J. 2008; 12(3):372–377. doi:10.1007/s10995-007-0245-910.1007/s10995-007-0245-9
17 Paterno MT, Van Zandt SE, Murphy J, Jordan ET. Evaluation of a student-nurse doula program: an analysis of doula interventions and their impact on labor analgesia and cesarean birth. J Midwifery Womens Health. 2012; 57(1):28–34. doi:10.1111/j.1542-2011.2011.00091.x10.1111/j.1542-2011.2011.00091.x
18 Thomas M-P, Ammann G, Brazier E, Noyes P, Maybank A. Doula services within a healthy start program: increasing access for an underserved population. Matern Child Health J. 2017; 21(Suppl 1):59–64. doi:10.1007/s10995-017-2402-010.1007/s10995-017-2402-0
19 US Department of Agriculture. 2010 Rural-Urban Commuting Area Codes. Rev ed. US Department of Agriculture; 2019.
20 World Health Organization. WHO Recommendations for Augmentation of Labour. World Health Organization; 2014.
21 Goer, H, Romano A. Optimal Care in Childbirth: The Case for a Physiologic Approach. Pinter & Martin; 2013.
22 Jones L, Othman M, Dowswell T, et al. Pain management for women in labour: an overview of systematic reviews. Cochrane Database Syst Rev. 2012; 2012(3):CD009234. doi:10.1002/14651858.CD009234.pub210.1002/14651858.CD009234.pub2
23 Moradi F, Aryankhesal A, Heidari M, Soroush A, Sadr SR. Interventions in reducing caesarean section in the world: a systematic review. Malays J Med Sci. 2019; 26(5):21–37. doi:10.21315/mjms2019.26.5.310.21315/mjms2019.26.5.3
24 Centers for Disease Control and Prevention. Number, rate, and standard error of all-listed surgical and nonsurgical procedures for discharges from short-stay hospitals, by selected procedure categories: United States, 2010. Published 2010. https://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberrate.pdfhttps://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberrate.pdf
25 National Partnership for Women & Families. Cesarean birth trends in the United States, 1989–2015. Published March 2017. https://nationalpartnership.org/wp-content/uploads/2023/02/cesarean-section-trends-1989-2014.pdfhttps://nationalpartnership.org/wp-content/uploads/2023/02/cesarean-section-trends-1989-2014.pdf
26 Chaillet N, Belaid L, Crochetière C, et al. Nonpharmacologic approaches for pain management during labor compared with usual care: a meta-analysis. Birth. 2014; 41(2):122–137. doi:10.1111/birt.1210310.1111/birt.12103
27 Zhang L, Troendle J, Branch DW, et al. The expected labor progression after labor augmentation with oxytocin: a retrospective cohort study. PLoS One. 2018; 13(10):e0205735. doi:10.1371/journal.pone.020573510.1371/journal.pone.0205735
28 Obstetric care consensus no. 1: safe prevention of the primary cesarean delivery. Obstet Gynecol. 2014; 123(3):693–711. doi:10.1097/01.AOG.0000444441.04111.1d10.1097/01.AOG.0000444441.04111.1d
29 Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2019. Natl Vital Stat Rep. 2021; 70(2):1–51.
30 Centers for Disease Control and Prevention. Natality Public Use User Guide. Published 2012. https://www.cdc.gov/nchs/nvss/dvs_data_release.htmhttps://www.cdc.gov/nchs/nvss/dvs_data_release.htm
31 Centers for Disease Control and Prevention. Results: breastfeeding rates. Published July 29, 2022. Accessed December 16, 2022. https://www.cdc.gov/breastfeeding/data/nis_data/results.htmlhttps://www.cdc.gov/breastfeeding/data/nis_data/results.html
32 MacDowell M, Glasser M, Fitts M, Nielsen K, Hunsaker M. A national view of rural health workforce issues in the USA. Rural Remote Health. 2010; 10(3):1531.
33 Stonehocker J, Muruthi J, Rayburn WF. Is there a shortage of obstetrician-gynecologists? Obstet Gynecol Clin North Am. 2017; 44(1):121–132. doi:10.1016/j.ogc.2016.11.00610.1016/j.ogc.2016.11.006
34 Eckert E. Preserving the momentum to extend postpartum Medicaid coverage. Womens Health Issues. 2020; 30(6):401–404. doi:10.1016/j.whi.2020.07.00610.1016/j.whi.2020.07.006
35 Strauss N, Giessler K, McAllister E. How doula care can advance the goals of the Affordable Care Act: a snapshot from New York City. J Perinat Educ. 2015; 24(1):8–15. doi:10.1891/1058-1243.24.1.810.1891/1058-1243.24.1.8
36 Jetty A, Jabbarpour Y, Pollack J, Huerto R, Woo S, Petterson S. Patient-physician racial concordance associated with improved healthcare use and lower healthcare expenditures in minority populations. J Racial Ethn Health Disparities. 2022; 9(1):68–81. doi:10.1007/s40615-020-00930-410.1007/s40615-020-00930-4
37 Shen MJ, Peterson EB, Costas-Muñiz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities. 2018; 5(1):117–140. doi:10.1007/s40615-017-0350-410.1007/s40615-017-0350-4
Notes
- Conflicts of Interest: The authors have no conflicts of interest to disclose.
Acknowledgments:
The staff and past presidents of DONA (Doulas of North America) International, especially Sunday Tortelli, CCE, CD(DONA), BDT(DONA), HBCE, LCCE, CLC.