Introduction
Across the globe, as per WHO data on September 23, 2022, 611, 421,786 confirmed cases were registered and 6,512,438 people died (WHO, 2022). In response to COVID-19 and to contain the spread of the virus, since January 2020, various countries imposed nationwide lockdowns and other containment measures (Shen et al., 2020). People and nations around the world have been significantly affected by the pandemic in terms of their psychology and health. Many shocks, traumas, terrors, anxieties, and sadness have been experienced by people, families, students, and communities (Pawar, 2020). Closure of schools, colleges, universities, and educational institutions was a critical measure taken during the great lockdown, leading to stress, anxiety, and a feeling of helplessness among the students (Singh et al., 2020; Sundarasen et al., 2020). Higher education institution (HEI) students are considered vulnerable to mental health problems such as higher levels of anxiety, depression, substance abuse, and eating disorders than the general population. The emotional and physical burden caused by the COVID-19 pandemic has amplified mental health problems (Browning et al., 2021; Rono, 2021).
During the COVID-19 lockdown, the student community reported a high prevalence of anxiety, depression, and insomnia (Alfawaz et al., 2021; Marelli et al., 2021; Wang et al., 2022). The worldwide closure of schools and educational institutions has impacted 80% of the student population (Ogunode, 2020; Sahu, 2020). Due to the rising concern over the pandemic, many universities postponed or canceled the campus activities such as workshops, conferences, sports meets, etc. Further, the studies transitioned from face-to-face to online teaching (Gewin, 2020). Empirical pieces of evidence found that college students were most affected by COVID-19 and the great lockdown. HEI students’ mental health was worst hit by the COVID-19-induced lockdown. Besides, the pandemic has caused a higher level of depression, financial insecurity, and stress.
According to the survey conducted by active minds with 2,000 college students in the United States of America, COVID-19 has negatively impacted the mental health of 80% of the students. Further, the pandemic has added more anxiety to the lives of 91% of the students, 81% reported disappointment and sadness, 80% experienced loneliness or isolation during the pandemic (Activeminds, 2020). Many students in China reported mild-to-severe anxiety due to the COVID-19 pandemic (Cao et al., 2020; Chen et al., 2020). Among 983 Malaysian students, 20.4% reported minimal-to-moderate, 6.6% marked-to-severe, and 2.8% reported extreme levels of anxiety during COVID-19. Universities’ closure has impacted the students’ mental health, academic, family, and economic and social life (Cao et al., 2020; Zhai & Du, 2020). Thousands of students were unable to return to the country in 2020 to begin their studies due to travel restrictions (O’Sullivan, Rahamathulla, & Pawar, 2020). The students with high-risk perceptions toward COVID-19 showed low academic performance. The risk perception may increase students’ anxiety, stress, and discomfort and, in turn, reduce their academic performance (Lee, Lim, Allen, & Choi, 2021).
Among the students, the impact of COVID-19 depends on various vulnerable factors such as current age, educational status, low economic status, pre-existing mental health problems, and fear of infection (Singh et al., 2020). Under normal circumstances, a high level of psychological distress is prevalent among college students, leading to poor academic interest and performance (Joseph Jeyaraj Swaminathan & Dellagiulia, 2018; March-Amengual et al., 2022; Pushparaj, 2019; Sharp & Theiler, 2018). There are educational issues caused by the closure of schools and educational institutions and the move to home learning, online learning, or distance learning (Cox, 2020). As a result, the shift to online teaching has exacerbated the students’ academic stress (Grubic, Badovinac, & Johri, 2020). Financial constraints, remote online learning, and uncertainty about future academic and career prospects are the major stress factors associated with psychological problems (Sundarasen et al., 2020). A higher level of psychological impact was found among female students and students from low socio-economic status, in poor or fair health, spending more time on screens and knowing someone in the family or community infected with COVID-19. Young students, students from low-income families, and with pre-existing health conditions were at high risk of mental health problems during the pandemic (Browning et al., 2021). Since the psychological impact of COVID-19 on students’ mental health is high in magnitude, government and educational institutions must provide comprehensive psychological intervention to vulnerable students. In this review, the authors will highlight the psychological impact of the COVID-19 outbreak on university/college students and its associated risk factors.
Review Methods
For the current analytical review, a systematic search was conducted on different search engines and journals of PubMed (Public/Publisher MEDLINE), PsycINFO, Scopus, Google Scholar, Elsevier, Springer, Web of Science, Nature, PLOS ONE, JAMA (Journal of the American Medical Association), Research Gate, and other databases from January 2020 to September 2022. The search terms used for the review were: “COVID-19 and Students,” “psychological impact on college students,” “mental health of students,” “depression,” “anxiety,” and “stress” with various permutations and combinations.
Study Selection and Eligibility Criteria
Each publication was screened based on titles and abstracts. Then, the full-text articles were reviewed to check whether they were eligible for inclusion. The inclusion criteria for the study were that (1) the study should be a cross-sectional study, (2) it should address the psychological impact of COVID-19 among university/college students and its associated risk factors, (3) it should use standardized scales for measurement, (4) it should be published in peer-review journals, and (5) it should be published during the period of January 2020 to September 2022. The exclusion criteria were (1) studies not in English, (2) non-peer-reviewed journals, (3) literature not related to search/keywords, and (4) papers published before and after the specific period of the study.
Data Extraction and Synthesis
The authors extracted the following information from the full text: authors and year of publication, the country in which the study was done, study design, sample size, instruments used, number of participants, the prevalence of symptoms of stress/anxiety/depression, and associated risk factors.
Results
Study Characteristics
A total of 122 pieces of literature were identified for this analytical review. Of those, 20 studies were excluded due to duplication. Sixty articles were removed based on the screening of titles and abstracts. Forty-two articles were accessed for eligibility and out of it 22 full-text articles were excluded (10 reviews, 7 qualitative studies, and 5 mixed-method studies). Hence, 20 studies met the inclusion criteria and were included in the review. Twenty cross-sectional studies were conducted in 12 countries, including the United States of America (n = 2), China (n = 1), Ethiopia (n = 1), Bangladesh (n = 3), Malaysia (n = 2), Greece (n = 1), Kosovo (n = 1), Egypt (n = 1), Jordan (n = 1), Pakistan (n = 1), Indonesia (n = 1), and India (n = 4). A variety of scales were used for measuring the psychiatric outcome of the studies (n = 20). The Depression, Anxiety and Stress Scale- 21 items (DASS-21), Perceived Stress Scale (PSS), Generalized Anxiety Disorder Scale- 7 (GAD-7), Positive and Negative Affect Schedule (PANS), Penn State Worry Questionnaire (PSWQ), Patient Health Questionnaire (PHQ), Zung’s self-rating anxiety scale (SAS), Subclinical Stress Symptom Questionnaire- 25 (SSQ-25), Beck Depression Inventory (BDI), Hospital Anxiety and Depression Scale (HADS), and Hamilton Anxiety Rating Scale (HAM-A) were used to assess the depression, anxiety, and stress symptoms. Impact of Event Scale-Revised (IES- R) was used to evaluate the degree of distress among students in response to the COVID-19 crisis, and the Multidimensional Scale of Perceived Social Support (MSPSS) was used to measure the social support received during the pandemic.
The Psychological Impact of COVID-19 on HEI Students
The COVID-19 pandemic and its subsequent lockdown caused unique mental health issues among HEI students. Health experts say that a healthcare crisis posed a dual challenge for both the mind and body. The worldwide closure of schools and educational institutions impacted 80% of the student population (Sahu, 2020). Fear of contracting the infection is one of the sources of stress among college students. The HEI students also experienced pandemic-related problems like disrupted social rhythms and daily routines. During the COVID-19 lockdown, the student community reported a high prevalence of anxiety, depression, and insomnia (Alfawaz et al., 2021). University students are considered vulnerable to various mental health problems (Pushparaj & Vinnarasi, 2019), such as higher levels of anxiety, depression, substance misuse, and eating disorders, as compared to the general population. The burden caused during the COVID-19 pandemic has amplified these mental health problems (Browning et al., 2021). A study from the United States of America directly reported the psychological impact of COVID-19 among university students. The findings showed that the psychological impact was high among female students. Besides, higher levels of psychological impact were found among the students who were non-Hispanic Asians, with fair/poor health status, between 18 and 24 years of age, spending more than 8 hours on screens every day, and knowing someone infected with the virus (Browning et al., 2021).
While analyzing some of the high-income economies, Table 1 exposes that the students’ mental health has been affected by COVID-19 experiences. These experiences are basically based on the effects of quarantine, social distance, academic delays, fear of infection, disruption of sleep, decreased social interaction, and increased time on screens.
High-income economies
| Author (Year) | Country | Sample size | Study design | Assessment tool | Prevalence rate (%) | Associated risk factors |
|---|---|---|---|---|---|---|
| Konstantopoulou, Pantazopoulou, Iliou, and Raikou (2020). | Greece | 1,140 University students | Cross-sectional | SSQ-25, BDI |
Anxiety: subclinical anxiety symptoms (68.0%) Depression: mild (28.2%) and moderate (32.3%) PTSD: 83.1% |
Quarantine and social distance |
| Khoshaim et al. (2020). | Saudi Arabia | 400 University students | Cross-sectional study | SAS | Anxiety: mild to moderate 86/400 (21.5%), marked to severe 35/400 (8.8%), and most extreme 17/400 (4.3%) | Female, age group (19–25 years), and level of education |
| Son, Hegde, Smith, Wang, and Sasangohar (2020). | United States of America | 195 College students | Cross-sectional | PSS | Stress & Anxiety: 138/195 (71%) Depression: 86/195 (44%) Suicidal thoughts: 16/195 (8%) |
Academic delays, fear of infection, disruption of sleep, and decreased social interaction |
| Browning et al. (2021). | United States of America | 2,140 University students | Cross-sectional | PANS, PSWQ |
Psychological impact: high 1,146/2,140 (45.2%), moderate 1,025/2,140 (40.4%), and low 363/2,140 (14.3%) | Female, non-Hispanic Asian, having fair/poor health, low family income, age group (18–24 years), spending more than 9 hours on screens, and having relatives or acquaintances infected with COVID-19 |
PANS, Positive and Negative Affect Schedule; PSWQ, Penn State Worry Questionnaire; SAS, Self-rating Anxiety Scale; PSS, Perceived Stress Scale; SSQ, Subclinical Stress Symptom Questionnaire; BDI, Beck Depression Inventory.
While investigating the impact of COVID-19 on the mental health of the students in some of the upper-middle-income economies, Table 2 reveals that the impact had been severe and the experiences of anxiety, depression, and stress were from mild to severe. They were induced by academic delays, economic stressors, frustration from loss of daily routine, disruption of study, quarantine, staying alone, remote learning, loneliness, and uncertainty related to academic performance, graduation, and future career prospects.
Upper middle-income economies
| Author (Year) | Country | Sample size | Study design | Assessment tool | Prevalence rate (%) | Associated risk factors |
| Cao et al. (2020). | China | 7,143 College students | Cross-sectional | GAD-7 | Anxiety: severe (0.9%), moderate (2.7%), and mild (21.3) | Having acquaintances infected with COVID-19, economic stressors, effects on daily life, and academic delays |
| Woon, Leong Bin Abdullah, Sidi, Mansor, and Nik Jaafar (2021). | Malaysia | 316 University students | Cross-sectional | MSPSS, DASS-21 |
Depression: mild 49/316 (15.5%), moderate 37/316 (11.7%), and severe 29/316 (9.2%). Anxiety: mild 22 (7.0%), moderate 42 (16.5%), and severe 42/316(13.2%). Stress: mild 83/316 (26.3%), moderate 30/316 (9.5%), and severe 21/316 (6.6%) |
Frustration from loss of daily routine, disruption of study, and history of psychiatric illness |
| Sundarasen et al. (2020). | Malaysia | 983 University students | Cross-sectional | SAS | Anxiety: minimal to moderate (20.4%), marked to severe (6.6%), and most extreme levels (2.8%) | Female gender, age group (19–25 years), staying alone, remote learning, uncertainty related to academic performance, graduation and future career prospects |
| Arënliu et al. (2021). | Kosovo | 904 University students | Cross-sectional | HADS | Depression: mild 167/904(18.5), moderate 71/904 (7.9%), severe 33/904(1.7%) Anxiety: mild 202/904 (22.4%), moderate 98/904 (10.9%), and severe 33/904 (3.7) |
Economic stress, seeking excessive information related to COVID-19, knowing relatives or friends infected with COVID-19, and loneliness |
| Hamaideh, Al-Modallal, Tanash, and Hamdan-Mansour (2022). | Jordan | 1,380 Jordanian university students | Cross-sectional | DASS-21 | Depression: 78.7% Anxiety: 67.9% Stress: 58.7% |
Distance learning, home quarantine, disturbances in sleeping and eating, afraid of academic grades, feeling loneliness, and family members with chronic illness |
DASS, Depression, Anxiety and Stress Scale; GAD, Generalized Anxiety Disorder Scale; SAS, Self-rating Anxiety Scale; HADS, Hospital Anxiety and Depression Scale; MSPSS, Multidimensional Scale of Perceived Social Support.
While investigating the impact of COVID-19 on the mental health of the students in some of the lower-middle-income economies, Table 3 reveals that in the high-income and upper-income economies, the impact had been the same, and the experiences of stress, anxiety, and depression were from mild to severe. They were caused by prolonged unemployment, financial insecurity, fear of infection, inadequate food supply, lack of social support, academic delays, lack of social interaction, worsening financial conditions, spending more time on mobiles, and concerns about future career prospects.
Lower middle-income economies
| Author (Year) | Country | Sample size | Study design | Assessment tool | Prevalence rate (%) | Associated risk factors |
|---|---|---|---|---|---|---|
| Islam, Barna, Raihan, Khan, and Hossain (2020). | Bangladesh | 476 University students | Cross-sectional | PHQ-9, GAD-7 |
Depression: mild to severe 392/476 (82.4%) Anxiety: mild to severe 389/476 (87.7%). |
Prolonged unemployment, financial insecurity, and concerns about the future career prospects |
| Khan, Sultana, Hossain, Hasan, Ahmed, and Sikder (2020). | Bangladesh | 505 College students | Cross-sectional | DASS-21, IES |
Depression: mild to extremely severe (46.92%) Stress: 28.5% Anxiety: 46.92% |
Financial uncertainty, fear of infection, inadequate food supply, and excessive exposure to COVID-19 news in social and mass media |
| Dhar, Ayittey, and Sarkar (2020). | Bangladesh | 15,543 University students | Cross-sectional | GAD-7 | Anxiety: severe (44.59%), moderate (48.41 %), and moderate mild (3.82%) | Economic stressors, academic delays, effects on daily life, and families or friends being infected with the epidemic, are positively related to anxiety and worry about the social support during COVID-19 |
| Ghazawy et al. (2021). | Egypt | 1,335 University students | Cross-sectional | DASS-21 | Depression: 70.5% Anxiety: 53.6% Stress: 47.8% |
Being a female, having a relative or acquaintance infected with COVID-19, having a preexisting chronic disease and lacking psychological support from families, community, and universities |
| Biswas and Biswas (2021). | India | 209 College students | Cross-sectional | GAD-7, HAM-A |
Anxiety: severe 3/209 (1.44%), moderately severe 30/209 (14.35%), moderate 76/209 (36.36%), and mild 100/209 (47.85%) | Female, academic delays, disruption of daily life, and lack of social support |
| Bijulakshmi, Ramasubramanian, Rajendhiran, and Ramasubramani (2020). | India | 775 College students | Cross-sectional | PSS | Perceived stress: low 57/775 (7.4%), moderate 629/775 (81.2%), and high 89/775 (11.5%) | Concerns regarding education, future career prospects, and reduced social interaction with friends or peers |
| Ravichandran, Palanichami, Kalaiselvan, Muthukumar, and Mahalingam (2020). | India | 727 College students | Cross-sectional | DASS-21 | Depression: mild 111/727 (15.2%), moderate 143/727 (19.7%), severe 66/727 (9.1), and extremely severe 66 (9.1) Anxiety: mild 58/727 (8%), moderate 117/727(16.1%), severe 45/727 (6.2%), and extremely severe 50/727 (6.9%) Stress: mild 63/727 (8.6%), moderate 62/727 (8.5%), severe 37/727 (5.1%), and extremely severe 15/727 (2.1%) |
Forcing the students to stay in the home, fear of infection, worsening financial conditions in the family, lifestyle changes, reduced contact with friends, and using mobile phones more than usual |
| Satpathy and Ali (2020). | India | 83 College students | Cross-sectional | DASS-21 | Depression: 43% Anxiety: 16% Stress: 11 % |
The economic downturn, concerns about the future, social distress, and future career prospects |
| Chakraborty, Subbiah, and Damade (2020). | India | 335 (168 Dental students & 167 practitioners) | Cross-sectional | PHQ | Depression: mild (34%), moderate (27%), and severe (27%) | Concerns about professional growth, afraid of contracting COVID-19 from clinical patients, and concerns about employment prospects |
DASS, Depression, Anxiety and Stress Scale; PSS, Perceived Stress Scale; GAD, Generalized Anxiety Disorder Scale; PHQ, Patient Health Questionnaire; HAM, Hamilton Anxiety Rating Scale; IES, Impact of Event Scale.
Depression
The prevalence of depression was reported in eight studies ranging from 21.2 to 82.4% among both university (Aylie, Mekonen, & Mekuria, 2020; Hamaideh et al., 2022; Islam et al., 2020; Woon et al., 2021) and college students, (Chakraborty et al., 2020; Ravichandran et al., 2020; Satpathy & Ali, 2020; Son et al., 2020) respectively. In a cross-sectional study among Bangladesh university students, 82% (n = 476) reported mild-to-severe depression. The authors highlighted that prolonged unemployment and financial uncertainties are the significant stress factors associated with depressive symptoms (Islam et al., 2020). About 50.2% out of 1,542 Saudi Arabian university students had depressive symptoms. Further, 65.3% of the students reported that their family bonds have got strengthened during the lockdown. Also, the authors suggest that strong family bonding is one of the students’ coping strategies during the pandemic (Dhar et al., 2020). The lowest prevalence rate (21.2%) was identified in Ethiopian university students compared to other studies in this review (Aylie et al., 2020). Among college students, 44% out of 195 reported increased levels of depressive thoughts in the United States of America (Son et al., 2020). Two Indian studies reported the prevalence of depressive symptoms among college students. In the first study, 53% (n = 727) of prevalence rates were identified (Ravichandran et al., 2020) and the second study reported 43% (n = 83) (Satpathy & Ali, 2020). A survey among dental college students (n = 335) in India reported mild (34%), moderate (27%), and severe (27%) levels of depressive symptoms. The factors attributed to higher depressive symptoms were concerns related to setbacks in clinical training, research experience, and fear of contracting COVID-19 viral infection during clinical postings (Chakraborty et al., 2020).
Anxiety
The prevalence of anxiety was reported in 12 studies that were included in the review (Aylie et al., 2020; Biswas & Biswas, 2021; Cao et al., 2020; Chinna et al., 2021; Dhar et al., 2020; Islam et al., 2020; Khan et al., 2020; Konstantopoulou et al., 2020; Ravichandran et al., 2020; Satpathy & Ali, 2020; Sundarasen et al., 2020; Khoshaim et al., 2020). The rates of symptoms of anxiety ranged from 3.82 to 87.7%. A cross-sectional study among college students (n = 7,143) in China reported severe (0.9%), moderate (2.7%), and mild (21.3%) levels of anxiety (Cao et al., 2020). This paper also identified the risk factors associated with anxiety symptoms such as low family income, disturbances in routine life, academic delays, and close friends and relatives infected with COVID-19 had increased the anxiety level. In a study among Bangladesh university students (n = 505), 33.3% showed anxiety symptoms. Further, the study suggests that excessive exposure to COVID-19 news on social media is one of the stress factors associated with a higher level of anxiety (Khan et al., 2020). Another study with Bangladeshi students (n = 15,543) reported severe (n = 44.5%), moderate (48.41%), and mild (3.82%) levels of anxiety. The results highlighted that the epidemic-related stress factors like concerns about academic delays (r = 0.321, p < 0.001) and social support (r = 0.321, p < 0.001) positively correlated with the students’ anxiety levels (Dhar et al., 2020). The lowest prevalence rate was identified in three studies, 21.3% (n = 7,143) in China (Cao et al., 2020), 27.7% (n = 322) in Ethiopia (Aylie et al., 2020) and 16% (n = 83) in India (Satpathy & Ali, 2020). Malaysian university students (n = 983) experienced minimal-to-moderate (20.4%), marked-to-severe (6.6%), and extreme (2.8%) levels of anxiety (Sundarasen et al., 2020). Also, it was found that remote online learning is one of the causative factors associated with a higher level of anxiety among Malaysian students (Sundarasen et al., 2020). The highest prevalence (87.7%) of anxiety levels was identified in Bangladeshi students (n = 476) (Islam et al., 2020), and also a high prevalence of moderate anxiety symptoms was identified in the university students of Greece (68%) (Konstantopoulou et al., 2020) in this review. A study among university students in seven Asian countries (Malaysia, Saudi Arabia, Pakistan, Bangladesh, China, India, and Indonesia) reported mild-to-moderate (21.9%) and severe-to-extreme (13.7%) levels of anxiety. Two Indian studies reported the prevalence of anxiety symptoms among college students with a rate of 37.2% (n = 727) in one study (Ravichandran et al., 2020), and in the other study (n = 209), severe (14.35%), moderate (36.36%), and mild (47.85%) prevalence rate of anxiety was identified (Biswas & Biswas, 2021). Also, the authors found that increased domestic violence in the family during the COVID-19 lockdown was associated with anxiety among Indian students (Biswas & Biswas, 2021).
Stress
The prevalence of stress was reported by six studies ranging from 11 to 81.2% in college (Bijulakshmi et al., 2020; Hamaideh et al., 2022; Khan et al., 2020; Ravichandran et al., 2020; Satpathy & Ali, 2020; Woon et al., 2021) and university students (Ghazawy et al., 2021). A cross-sectional study among college students (n = 775) in India reported moderate (81.2%) and high levels (11.5%) of stress. This paper also identified that limited contact with peers during the pandemic is one of the causative factors of stress among Indian students. A prevalence rate of 47.8% out of 1,335 students was found among university students in Egypt. Also, the authors pointed out that the risk factors associated with stress among Egyptian students are a lack of psychological support from the family, community, and university (Ghazawy et al., 2021). About 28.5% (n = 505) of the prevalence rate was identified in Bangladeshi college students (Khan et al., 2020). Reasons for this include absence of physical exercise, limited recreational activity, inadequate food supply, lack of information about COVID-19, and more exposure to COVID-19 news. Two Indian studies reported the lowest stress prevalence rate 24.3% (n = 727) (Ravichandran et al., 2020) and 11% (n = 516) (Satpathy & Ali, 2020).
Risk factors of psychological problems
Socio-demographic factors
Age
Six studies identified the significant risk factors for psychological problems among students. A higher level of psychological impact was predicted in the age group of 18–24 years (Browning et al., 2021; Wathelet et al., 2020). Students in their early 20s reported higher levels of depressive symptoms (Islam et al., 2020) and anxiety (Biswas & Biswas, 2021; Sundarasen et al., 2020). But, two studies reported a higher level of psychological impact in students older than 25 years (Khan et al., 2020; Konstantopoulou et al., 2020).
Gender
The association between gender and mental health problems was identified in 13 studies, the female students reported significantly higher average scores for depression, anxiety, and stress than their male counterparts (Arënliu et al., 2021; Aylie et al., 2020; Biswas & Biswas, 2021; Browning et al., 2021; Ghazawy et al., 2021; Salman et al., 2022; Wathelet et al., 2020). The odds of anxiety among female students were found to be higher than the male students (Sundarasen et al., 2020). Similar stress scores were identified in both male and female students in China (Cao et al., 2020). In contrast, the male students (67.35%) in Bangladesh reported higher levels of depressive symptoms than their female (32.65%) counterparts (Islam et al., 2020) and they were more severely worried than the female during the COVID-19 pandemic (Dhar et al., 2020). A statistically significant association was not observed between the gender and subclinical symptoms of anxiety and traumatic stress among university students in Greece (n = 1,140) (Konstantopoulou et al., 2020).
Income
Lower family income during the COVID-19 pandemic was found to be associated with a high risk of mental health problems among the students. Eight studies identified financial stress as a significant factor that contributes to higher levels of depression, anxiety, and stress symptoms in students (Aylie et al., 2020; Browning et al., 2021; Cao et al., 2020; Dhar et al., 2020; Islam et al., 2020; Khan et al., 2020; Satpathy & Ali, 2020; Sundarasen et al., 2020).
History of Medical Illness
Students with a history of medical illness have reported a higher level of depression, anxiety, and stress symptoms during the COVID-19 pandemic due to compromised immunity caused by pre-existing conditions (Corse et al., 2020). Two studies have identified that university/college students with a history of medical/psychiatric illnesses have a chance of developing a higher level of depression, anxiety, and stress symptoms (Aylie et al., 2020; Ghazawy et al., 2021). Further, having a poor/fair general health status was found to be associated with higher levels of psychological impact (Browning et al., 2021) during the COVID-19 outbreak.
Psychological and Social Factors
Two studies reported that the COVID-19 pandemic has led to increase fear among students (Khan et al., 2020). Fear of contracting COVID-19 infection had a significant association with depression, anxiety, stress, and post-traumatic symptoms (Khan et al., 2020). Also, a higher level of depressive symptoms was observed in Indian dental students who were afraid of contracting COVID-19 during clinical postings. Sleep disturbance during the COVID-19 lockdown was reported by Saudi Arabian university students (n = 1,542) (Alfawaz et al., 2021) and college students in the United Kingdom (n = 195) (Son et al., 2020). Three studies reported that the closure of colleges and universities has reduced social interaction with peers, and induced psychological distress among students (Ravichandran et al., 2020; Son et al., 2020). Academic delay due to lockdown was found to be positively correlated with anxiety symptoms (Biswas & Biswas, 2021; Dhar et al., 2020), and increased concerns about academic performance were identified in two studies (Son et al., 2020; Sundarasen et al., 2020). Having relatives or acquaintances infected with COVID-19 predicted higher levels of psychological impact (Browning et al., 2021), anxiety (Arënliu et al., 2021; Cao et al., 2020), and depression (Arënliu et al., 2021). Lack of social support from families, communities, and educational institutions during the lockdown also increased the risk of depression (Aylie et al., 2020), anxiety (Aylie et al., 2020; Biswas & Biswas, 2021; Dhar et al., 2020), and stress (Aylie et al., 2020). Three studies have found a strong link between excessive social media exposure and psychological problems (Arënliu et al., 2021; Browning et al., 2021; Khan et al., 2020). Learning through online platforms has given rise to the prevalence of anxiety (Arënliu et al., 2021; Sundarasen et al., 2020), depression (Arënliu et al., 2021), and stress. Further, excessive use of mobile phones more than usual during the lockdown was found to be associated with negative emotions, and they were identified in two studies (Browning et al., 2021; Ravichandran et al., 2020). Students’ concerns about their future career prospects were found to be associated with a higher level of anxiety (Sundarasen et al., 2020), perceived stress (Ravichandran et al., 2020), and psychological distress (Satpathy & Ali, 2020). One study with college students in the United States of America reported increased rates of suicidal thoughts during the COVID-19 pandemic (Son et al., 2020).
Discussion
The current review explored the psychological impact of COVID-19 on university/college students and its predictive factors. In general, there is an increased prevalence of psychiatric symptoms among students compared to their prevalence before the pandemic (Huang et al., 2019). The prevalence rate of depression, anxiety, and stress ranges from 21.2 to 82.4%, 3.82 to 87.7%, and 11 to 81.2%, respectively. Variations in the prevalence rate were found in the studies, which could be due to various tools used for measurement, cutoff scores of the instruments, reporting patterns, cultural differences, social support systems, the infection rate in the study area, etc. The regional difference was observed in the prevalence of mental health problems among the students during the outbreak of COVID-19, which could have resulted from the availability of health infrastructure, quality of governance, economy, policy response, and dissemination of information during the COVID-19 crisis. However, the issues mentioned above were not identified in the studies during the review, limiting the findings’ generalizability. Several contributing factors were also identified in the review. For example, the female students reported a significant increase in the level of depression, anxiety, and stress symptoms during the pandemic compared to their male counterparts (Arënliu et al., 2021; Aylie et al., 2020; Biswas & Biswas, 2021; Browning et al., 2021; Ghazawy et al., 2021; Salman et al., 2022; Wathelet et al., 2020). A higher level of psychological impact was predicted in the age group of 18–24 years (Browning et al., 2021; Wathelet et al., 2020). Further, students in their early 20s reported a higher level of depressive symptoms (Islam et al., 2020), and anxiety (Biswas & Biswas, 2021; Sundarasen et al., 2020), due to the closure of educational institutions.
Students with a history of medical illness have reported a higher level of depression, anxiety, and stress symptoms during the COVID-19 pandemic due to compromised immunity caused by pre-existing conditions (Aylie et al., 2020; Corse et al., 2020; Ghazawy et al., 2021). Having a poor/fair general health status was found to be associated with higher levels of psychological impact (Browning et al., 2021). This could be due to the postponement of treatment and lack of access to medical services during the COVID-19 pandemic. Additionally, during the pandemic, external stress factors like social isolation lead to loneliness and boredom have a significant effect on the physical and mental health of the students. Many studies have identified a strong link between excessive social media exposure and psychological problems (Arënliu et al., 2021; Browning et al., 2021; Khan et al., 2020). Seeking more COVID-19-related information through social and mass media has amplified anxiety and stress levels among students (Khan et al., 2020). Further, fake news reported on social media is one of the causative factors for stress and anxiety. Studies have reported that learning through online platforms has given rise to the prevalence of anxiety, stress, and depressive symptoms (Arënliu et al., 2021; Sundarasen et al., 2020). In addition, the abrupt switch from traditional face-to-face to online learning likely diminishes students’ academic motivation as they face additional self-regulated learning challenges (Sukhawathanakul, Hadwin, Rostampour, Bahena Olivares, & Shostak, 2022). Online learning has disrupted the students’ social lives with their peers in university/college and has led to social isolation. Further, excessive use of mobile phones than usual during the lockdown was associated with negative emotions (Browning et al., 2021; Ravichandran et al., 2020). Closure of colleges/universities has reduced students’ contact with their friends, and induced psychological distress reported in many countries (Ravichandran et al., 2020; Son et al., 2020). Studies have suggested that lower family income, academic delays, and increased concerns about academic performance and career prospects were found to be associated with a higher level of anxiety, perceived stress, and psychological distress during the pandemic (Aylie et al., 2020; Browning et al., 2021; Cao et al., 2020; Dhar et al., 2020; Khan et al., 2020; Ravichandran et al., 2020; Satpathy & Ali, 2020; Sundarasen et al., 2020). Studies also identified that poor social support from families, society, and educational institutions; having relatives and friends being infected with the pandemic; fear of contracting the COVID-19 virus; losing part-time jobs, prolonged unemployment, financial uncertainty, inadequate food supply, and lack of physical exercise are the significant predictors for developing psychological symptoms (Islam et al., 2020; Khan et al., 2020).
The findings indicate that educational institutions should consider providing psychological support to the most vulnerable students by embarking on structured programs like life-skills training and mindfulness therapy to reduce anxiety levels; providing psychological-oriented services to mitigate the emotional impact of the outbreak; staying connected with students using social media platform and motivating them to move forward during the crisis; training the educators in basic aspects of students mental health care; educating the students about the psychological effects of COVID-19 pandemic along with multidimensional psychological interventions like Cognitive Behavioural Therapy (CBT), psycho-education, behavioral activation; (Arënliu et al., 2021; Aylie et al., 2020; Chakraborty et al., 2020; Ghazawy et al., 2021; Sundarasen et al., 2020). Individuals’ efforts like regular physical activity, maintaining healthy dietary habits, interacting with family members, focusing on healthy lifestyle changes, relying on trusted sources of information related to the COVID-19 pandemic, using Internet sites effectively and avoiding excessive exposure to media coverage can help students to deal with the negative psychological impact of the COVID-19 pandemic (Adefris & Moges, 2021; Biswas & Biswas, 2021; Carek, Laibstain, & Carek, 2011; Dhar et al., 2020; Pushparaj et al., 2022). Further, academic institutions must re-evaluate curriculums, learning outcomes, and evaluation strategies to provide effective online courses.
Universities must prioritize mental health awareness to empower students during such disasters. Higher education should continue providing counseling to their students (tele-mental health counseling). Since tele-mental health counseling has been shown to be effective in treating anxiety and depressive symptoms (Brenes, Danhauer, Lyles, Hogan, & Miller, 2015), implementing it will facilitate counseling services to address students’ pressing mental health concerns. Students can also join online support groups to share their concerns and seek social support through counseling centers (Rollman et al., 2018). Furthermore, university counseling centers and other departments should disseminate public health messages to students and provide them with the necessary skills to preserve their mental health.
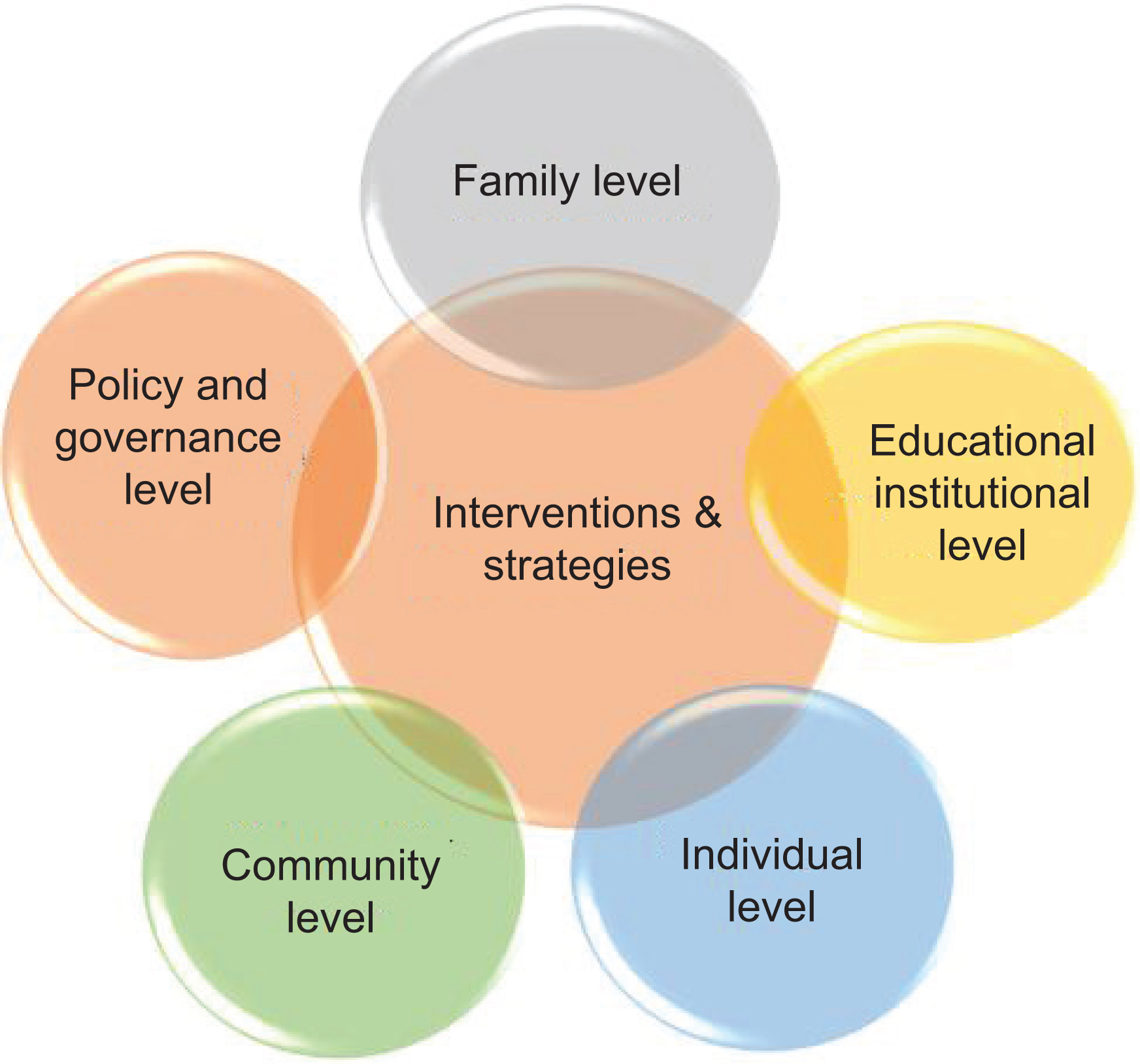
Interventions and Strategies
The interventions and strategies to help HEI students to overcome the psychological impacts during the multiple waves of COVID-19 need to be addressed at three levels: at the individual level, family level, and educational institutional level (Figure 1).
Interventions at Individual Level
At the individual level, the students can adopt to any one or two strategies proposed in Table 4.
Interventions and strategies at individual level
| Yoga (Nagendra, 2020) |
| Meditation (Pushparaj et al., 2022) |
| Mindfulness activities (Koner & Weaver, 2021) |
| Building resilience (Giordano et al., 2022) |
| Self-care practices (Brouwer et al., 2021) |
| Being optimistic (Arslan & Yıldırım, 2021) |
| Maintaining positive thoughts and being cheerful (Bakioğlu et al., 2021) |
| Practicing self-compassion (Gutiérrez-Hernández et al., 2021) |
Most of the strategies suggested here are very easy to adopt and practice even in the worst situations like COVID-19. Yoga and meditation (Nagendra, 2020; Pushparaj et al., 2022) are the most important and effective strategies to follow. This can be learned even through social media platforms if someone is a beginner. Learning and doing mindfulness activities (Koner & Weaver, 2021) and self-care practices (Brouwer et al., 2021) help one to overcome the challenges of mental health.
Building resilience in oneself helps to improve one’s well-being (Giordano, Cipolla, & Ungar, 2022). Optimism is one of the important virtues required for everyone. It helps in overcoming psychological stress in life and to find meaning in life (Arslan & Yıldırım, 2021). It is very important to keep oneself cheerful and to develop a sense of humor to enhance one’s well-being (Saricali, Satici, Satici, Gocet-Tekin, & Griffiths, 2022). Maintaining positive thoughts (Bakioğlu, Korkmaz, & Ercan, 2021) and practicing self-compassion helps one to improve his/her well-being (Gutiérrez-Hernández et al., 2021).
Interventions at the Family Level
Family plays an important role in enhancing the overall well-being of students. During the COVID-19 lockdown, the family members got the chance to spend more time with each other (Table 5).
Interventions and strategies at family level
| Strengthening family bonds (Alfawaz et al., 2021) |
| Forgiving people (Ciencia et al.; Pushparaj et al., 2022) |
| Being kind to people (Symeonidou et al., 2019) |
| Building family resilience (De Rosa & Rizzolli, 2021) |
Family bonding is identified as one of the coping mechanisms to preserve mental well-being (Alfawaz et al., 2021). Family bonding plays a vital role in overcoming psychological distress (Avasthi, 2010). Helping the students to forgive people who have hurt them in one way or the other helps them to overcome bitter feelings and to improve their overall well-being (Ciencia, Barry, & Toussaint; Pushparaj et al., 2022).
Helping students to practice kindness to themselves and to others is one of the wonderful gifts a family can instill in the lives of young people (Symeonidou, Moraitou, Pezirkianidis, & Stalikas, 2019). As a family, it is important that it builds up their resilience by strengthening the bond among them and enjoy the presence of each other and bases itself on a good value system and builds up strong communication among the family members (De Rosa & Rizzolli, 2021; Gayatri & Irawaty, 2022).
Interventions at HEIs Level
Educational institutions have a greater responsibility of taking care of their students in situations like the COVID-19 pandemic. Most of the institutions found innovative ways to connect to their students and helped them (Table 6).
Interventions and strategies at HEIs level
| Providing life skills training (Sundarasen et al., 2020) |
| Providing mindfulness therapy (Sundarasen et al., 2020) |
| Providing psychological help and orientation (Aylie et al., 2020; Cao et al., 2020) |
| Connecting the students through social media platforms (Islam et al., 2020) |
| Motivating them through webinars (Q. Li et al., 2021) |
| Educating them about the effects and facts of COVID through online mode (Chrikov et al., 2020; Islam et al., 2020) |
| Building social support (F. Li et al., 2021) |
| Encouraging them for regular physical activities (Adefris & Moges, 2021) |
| Educating them on healthy lifestyle (Adefris & Moges, 2021) |
| Providing tele-counseling help to the students (Chrikov et al., 2020) |
Six studies from Saudi Arabia have directly addressed the universities’ role in providing psychological support to students (Arënliu et al., 2021; Aylie et al., 2020; Cao et al., 2020; Chakraborty et al., 2020; Ghazawy et al., 2021; Sundarasen et al., 2020). In addition, two studies have examined the crucial role of the government to address the mental health concerns of university/college students during the COVID-19 crisis, such as developing health system strategies to provide crisis-oriented psychological services (Aylie et al., 2020) and working closely with the university to deliver economic psychological support (Islam et al., 2020). Several studies have addressed the following intervention strategies for universities/colleges to support vulnerable students during COVID-19: (1) embarking on structured programs like life skills training and mindfulness therapy to reduce anxiety levels (Sundarasen et al., 2020); (2) providing psychological services to mitigate the emotional impact of the outbreak (Browning et al., 2021; Ghazawy et al., 2021); (3) staying connected with students using social media platform and motivating them to move forward during the crisis (Islam et al., 2020); and (4) educating the students about the psychological effects of COVID-19 pandemic along with multidimensional psychological interventions like CBT, psycho-education, behavioural activation, etc. to cope with the current crisis (Khan et al., 2020). The importance of social support during the COVID-19 crisis was addressed in two studies (Biswas & Biswas, 2021). Further, a study from Ethiopia has discussed the following strategies that can help students to deal with the negative psychological impact of the COVID-19 pandemic: regular physical activity, interacting with family members, focusing on healthy lifestyle changes, relying on trusted sources of information related to the COVID-19 pandemic, using Internet sites effectively and avoiding excessive exposure to media coverage (Adefris & Moges, 2021).
Interventions at Community Level
Interventions at the community level are very important for the students with mental health issues (Table 7).
Interventions and strategies at community level
| Providing community mental health care (Iheanacho et al., 2015) |
| Providing education on mental health (Bourns & Holt, 2003) |
| Providing support system (Bourns & Holt, 2003) |
| Organizing sports (Appelqvist-Schmidlechner et al., 2018; Wang & Xing, 2022) |
| Organizing cultural events (Cohen et al., 2007) |
One of the important interventions at the community level is to provide mental health services to community members. It helps to screen people and to identify early signs and symptoms of mental health issues (Iheanacho et al., 2015).
It also helps in educating the community members about mental health issues and to come out with community-level strategies to promote positive mental health. Wherever it is required, the community can provide a support system to take care of their members’ mental health (Bourns & Holt, 2003).
The community can provide commonplace/gym to do physical exercises and can organize several sports activities to keep the youth active and to promote positive mental health (Appelqvist-Schmidlechner et al., 2018; Wang & Xing, 2022). The community can also organize several creative cultural events to keep the community together and to promote positive mental health (Cohen et al., 2007; Kading et al., 2015).
Interventions at Policy and Governance Level
Interventions at the policy and governance level are very important to promote positive mental health (Table 8).
Interventions and strategies at policy and governance level
| Coming up with creative programs and initiatives and to implement them at all HEI (Palaniswamy, 2022) |
| Creating a separate center under health department to promote positive mental health (Palaniswamy, 2022) |
| Providing more training to mental health professionals and to appoint them in every HEI (Palaniswamy, 2022) |
| Creating national-, state-, district-level mental resource centers (Johnson et al., 2022; Teachman et al., 2022) |
| Promoting and supporting digital technology-based help applications to promote positive mental health (Johnson et al., 2022; Teachman et al., 2022) |
Note: HEI, Higher Educational Institutions.
At the policy and governance level, there is a need to come up with lots of creative programs and initiatives. These initiatives need to be promoted and implemented at all the HEI. In order to give due importance to mental health, a separate center under the health department to promote mental health has to be created. This center should conduct trainings, courses to train mental health professionals and appoint them in every HEI (Palaniswamy, Panneer, Pushparaj, & Rose, 2022).
There should be a resource center at national, state, and district levels to address mental health issues and to promote positive mental health. The government should appreciate and promote digital technology-based applications to promote positive mental health (Johnson, Sanghvi, & Mehrotra, 2022; Teachman, Silverman, & Werntz, 2022).
Suggestions and Way Forward
Every university/college should add to their curriculum a course on positive mental health for all the students. The promotion of positive mental health activities needs to be encouraged both for faculties and students. It would be more appropriate to have a center in every HEI to promote human happiness and positive mental health.
Conclusion
This analytical review has examined the psychological impact of the COVID-19 pandemic on HEI students and its associated factors. The COVID-19 pandemic has impacted the lives of students in both industrialized and emerging economies. The findings of the review show that the psychological impact of COVID-19 on the mental health of the students is high in magnitude. Thus, considering the adverse psychiatric outcome, it is imperative that HEI must provide comprehensive psychological intervention to vulnerable students. The review has also presented a list of interventions to be used at various levels to help the HEI students. The review has also presented key strategies to follow as a way forward and voices for multi-stakeholder participation to help the HEI students. Considering the risk and protective factors, the government, educational institutions, and policymakers need to work closely to address the mental health needs of students during the pandemic crisis and beyond.
Author Contributions
S.P., S.D., and U.P, conceptualized the study. The methodology was determined by S.P., U.P., R.R.B.P., and S.P.1. Data analysis and data synthesis was done by S.P., U.P., S.P.1., J.S.R., and R.R.B.P. The original draft was prepared by S.P., S.D., U.P., and R.R.B.P. Review and editing of the original draft was done by S.P., U.P., S.P.1., J.S.R., and R.R.B.P. Visualization and supervision was done by S.P., S.D., and U.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
Activeminds. (2020). The impact of COVID-19 on student mental health. Retrieved July 9, 2021 from https://www.activeminds.org/studentsurvey/https://www.activeminds.org/studentsurvey/
Adefris, D., & Moges, B. (2021). The psychological impact and coping of COVID-19 pandemic among Arsi University students-Ethiopia. Current Psychology, https://doi.org/10.1007/s12144-021-01886-2https://doi.org/10.1007/s12144-021-01886-2
Alfawaz, H. A., Wani, K., Aljumah, A. A., Aldisi, D., Ansari, M. G. A., Yakout, S. M., … & Al-Daghri, N. M. (2021). Psychological well-being during COVID-19 lockdown: Insights from a Saudi State University’s Academic Community. Journal of King Saud University – Science, 33(1), 101262. https://doi.org/10.1016/j.jksus.2020.101262https://doi.org/10.1016/j.jksus.2020.101262
Al Mamun, F., Hosen, I., Misti, J. M., Kaggwa, M. M., & Mamun, M. A. (2021). Mental disorders of Bangladeshi students during the COVID-19 pandemic: A systematic review. Psychology Research and Behavior Management, 14, 645–654. https://doi.org/10.2147/prbm.S315961https://doi.org/10.2147/prbm.S315961
Appelqvist-Schmidlechner, K., Vaara, J., Häkkinen, A., Vasankari, T., Mäkinen, J., Mäntysaari, M., & Kyröläinen, H. (2018). Relationships between youth sports participation and mental health in young adulthood among Finnish males. American Journal of Health Promotion, 32(7), 1502–1509. https://doi.org/10.1177/0890117117746336https://doi.org/10.1177/0890117117746336
Arënliu, A., Bërxulli, D., Perolli-Shehu, B., Krasniqi, B., Gola, A., & Hyseni, F. (2021). Anxiety and depression among Kosovar university students during the initial phase of outbreak and lockdown of COVID-19 pandemic. Health Psychology and Behavioral Medicine, 9(1), 239–250. https://doi.org/10.1080/21642850.2021.1903327https://doi.org/10.1080/21642850.2021.1903327
Arslan, G., & Yıldırım, M. (2021). Coronavirus stress, meaningful living, optimism, and depressive symptoms: A study of moderated mediation model. Australian Journal of Psychology, 73(2), 113–124. https://doi.org/10.1080/00049530.2021.1882273https://doi.org/10.1080/00049530.2021.1882273
Avasthi, A. (2010). Preserve and strengthen family to promote mental health. Indian Journal of Psychiatry, 52(2), 113. https://doi.org/10.4103%2F0019-5545.64582https://doi.org/10.4103%2F0019-5545.64582
Aylie, N. S., Mekonen, M. A., & Mekuria, R. M. (2020). The psychological impacts of COVID-19 pandemic among university students in Bench-Sheko Zone, South-west Ethiopia: A community-based cross-sectional study. Psychology Research and Behavior Management, 13, 813. https://doi.org/10.2147/PRBM.S275593https://doi.org/10.2147/PRBM.S275593
Bakioğlu, F., Korkmaz, O., & Ercan, H. (2021). Fear of COVID-19 and positivity: Mediating role of intolerance of uncertainty, depression, anxiety, and stress. International Journal of Mental Health and Addiction, 19(6), 2369–2382. https://doi.org/10.1007/s11469-020-00331-yhttps://doi.org/10.1007/s11469-020-00331-y
Bijulakshmi, P., Ramasubramanian, V., Rajendhiran, G., & Ramasubramanian, C. (2020). Psychological impact of COVID 19 on the amount of perceived stress among college students studying across various streams in India during the period of lockdown. Journal of Evolution of Medical and Dental Sciences, 9(39), 2889–2894. https://doi.org/10.14260/jemds/2020/632https://doi.org/10.14260/jemds/2020/632
Biswas, S., & Biswas, A. (2021). Anxiety level among students of different college and universities in India during lock down in connection to the COVID-19 pandemic. Journal of Public Health (Berl.) 31, 49–55 (2023). https://doi.org/10.1007/s10389-020-01431-8https://doi.org/10.1007/s10389-020-01431-8
Bourns, N., & Holt, G. (2003). Community mental health and support services. In Mental health, intellectual disabilities, and the aging process (pp. 197–213). Ed: P.W. Davidson, V.P. Prasher and M.P. Janicki https://doi.org/10.1002/9780470776179.ch14